M. Sri Nithya
Roll. No 86
Patient came with the complaints of shortness of breath since 15 days
B/ l pedal edema and facial puffiness since 3 days
Burning micturition and decreased urine output since 2 days
Patient was apparently asymptomatic
5 months ago then he developed shortness of breath and visited local doctor and took treatment and then it subsided. Now patient presented with shortness of breath since 15 days, insidious in onset and gradually progressive from grade 1 to grade 3.
Orthopnea present, no PND
No h/o chest pain, palpitations , excessive sweating, giddiness, vomiting.
B/l pedal edema,pitting type, extending up to the knee joint present and facial puffiness present since 3 days
Burning micturition and decreased urine output since 2 days
No h/o fever, cough, cold, vomitings or loose motions
K/c/ o type 2 diabetes mellitus since 6 years on tablet metformin 500 mg po/od
K/c/o HTN since 8 years on tablet metoprolol 0.25 mg po/od
H/o CVA 8 years ago ?TIA took medications for 2 months and stopped.
Tab. Hydralazine 37.5 mg , Rosuvastatin 10 mg and clopidogrel
Dytor plus 5 mg
K/c/o alcoholic stopped since 2 years.
Stopped smoking since 6 years
On general examination-
Patient is conscious, coherent, cooperative
There is no pallor, icterus, cyanosis, clubbing, lymphadenopathy
B/l Pedal edema present ,pitting type,extending up to the knee joint
Vitals-
Temp-96. 8F
PR -70 bpm
RR -20 cpm
Bp-130/90 mmhg
Spo2-87% at RA, 100% at 4 lit of O2
Grbs- 186 mg/dl
CVS - S1,S2 present
RS- BAE+, NVBS
Dyspnea present, wheeze present bilaterally
Crepts +
P/A - normal
CNS-
GCS-E4V5M6
Reflexes- Right. Left
Biceps. 2+. 2+
Triceps. 1+. 1+
Supinator. 1+. 1+
Knee. 2+. 2+
Ankle. 1+. 1+
Diagnosis - Cardiogenic pulmonary edema (secondary to Heart failure with preserved ejection fraction)?UTI? Renal AKI on CVD with? Severe Anemia ? Nutritional. K/c/o type 2 DM, HTN
Treatment given-
Inj. Lasix 40 mg iv stat given
Inj. Hai s/c 7 point profile
Tab. Ecospirin Av 78/10 mg OD HS
Tab. Metoprolol 25 mg OD
O2 supplementation to maintain spo2- >94 %
Intermittent CPAP
MONITOR VITALS AND INFORM SOS
BP monitoring 4 th hourly
Investigations -
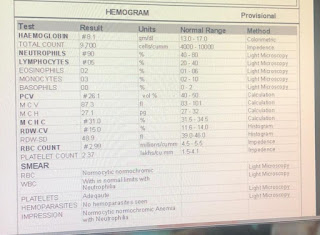
Hb-4. 7 g/dl
Tlc- 10,700
Neu-87
Lymphocytes -07
Pcv-17. 9
Mcv-65. 6
Mch- 17.2
Mchc-26. 3
Rdw-23. 7
RBC-2. 73
PLC- 4.24
BGT- O POSITIVE
BUN-14. 9
Reticulocyte count- 0.5
S. Magnesium - 1.8
S electrolytes-
Na- 135
K-3. 6
Cl-101
Ca2+- 1.10
B. UREA-32
S creat-1. 6
Rbs-86 mg/dl
Serology - negative
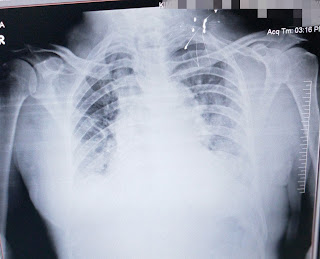
Chest xray-
ECG-
21/2/23
Ecg-22/2/23
ICU BED NO-2
UNIT-2
DOA-21/2/23
Patient came with the complaints of shortness of breath since 15 days
B/ l pedal edema and facial puffiness since 3 days
Burning micturition and decreased urine output since 2 days
S-
No fever spikes yesterday
1 unit PRBC transfusion done
O-
Patient is conscious, coherent, cooperative
Vitals-
Temp-99.2F
PR -62 bpm
RR -26cpm
Bp-150/80 mmhg
Spo2- 100% at 2 lit of O2
Grbs- 114 mg/dl
CVS - S1,S2 present
RS- BAE+, NVBS
Crepts + IAA, ISA (b/l)
P/A - soft, non tender, tympanic note present
CNS-
GCS-E4V5M6
Reflexes- Right. Left
Biceps. 2+. 2+
Triceps. 1+. 1+
Supinator. 1+. 1+
Knee. 2+. 2+
Ankle. 1+. 1+
Investigations -
Hb-4. 7 g/dl
Tlc- 10,700
Neu-87
Lymphocytes -07
Pcv-17. 9
Mcv-65. 6
Mch- 17.2
Mchc-26. 3
Rdw-23. 7
RBC-2. 73
PLC- 4.24
BGT- O POSITIVE
BUN-14. 9
Reticulocyte count- 0.5
S. Magnesium - 1.8
S electrolytes-
Na- 135
K-3. 6
Cl-101
Ca2+- 1.10
B. UREA-32
S creat-1. 6
Rbs-86 mg/dl
Serology - negative
ABG-
Ph-7. 489
Po2- 47.9
Pco2-32. 2
Hco3- 25.5
Na- 128
K-2. 5
Ca-0. 43
Cl-91
Lft-
Total bilirubin-0. 80
Direct-0. 19
Ast- 36
Alt-33
Alp-404
T. Proteins-5. 8
Albumin-3. 19
A/G -1.22
A-
Diagnosis - Cardiogenic pulmonary edema (secondary to Heart failure with preserved ejection fraction)?UTI? Renal AKI on CVD with? Severe Anemia ? Nutritional. K/c/o type 2 DM, HTN
P-
Inj. Lasix 40 mg iv bd
Inj. Hai s/c 7 point profile
Tab. Ecospirin Av 78/10 mg OD HS
Tab. Metoprolol 25 mg OD
Nebulisation with ipravent 12 th hourly
Budecort 12 th hourly
O2 supplementation to maintain spo2- >94 %
Intermittent CPAP
MONITOR VITALS AND INFORM SOS
BP monitoring 4 th hourly
23/2/23
ICU BED NO-2
UNIT-2
DOA-21/2/23
Patient came with the complaints of shortness of breath since 15 days
B/ l pedal edema and facial puffiness since 3 days
Burning micturition and decreased urine output since 2 days
S-
c/o sob decreased
No fever spikes yesterday
Stools not passed
2units PRBC transfusion done
O-
Patient is conscious, coherent, cooperative
Vitals-
Temp-97.6F
PR -73 bpm
RR -20cpm
Bp-150/80 mmhg
Spo2- 99% at 1 lit of O2
Grbs- 93 mg/dl 4 u hai given
On 21/2/23
8pm- 137 mg/dl
2am-137 mg/dl
On 22/2/23
8 am - 114 mg/dl
2pm- 135 mg/dl inj. Hai 4 u given
8pm- 72 mg/dl
On 23/2/23
2 am - 125 mg/dl
CVS - S1,S2 present
RS- BAE+, NVBS
P/A - soft, non tender, tympanic note present
CNS-
GCS-E4V5M6
Reflexes- Right. Left
Biceps. 2+. 2+
Triceps. 1+. 1+
Supinator. 1+. 1+
Knee. 2+. 2+
Ankle. 1+. 1+
Investigations -
Hb-7.6 g/dl
Tlc- 14100
Neu-80
Lymphocytes -15
Pcv- 25.9
PLC- 3.7
BGT- O POSITIVE
S electrolytes-
Na- 144
K-3. 2
Cl-100
Ca2+- 1.05
B. UREA-40
S creat-1. 7
22/2/23
Serology - negative
ABG-
Ph-7. 489
Po2- 47.9
Pco2-32. 2
Hco3- 25.5
Na- 128
K-2. 5
Ca-0. 43
Cl-91
Lft-
Total bilirubin-0. 80
Direct-0. 19
Ast- 36
Alt-33
Alp-404
T. Proteins-5. 8
Albumin-3. 19
A/G -1.22
Chest xray AP view
Chest xray PA view-
A-
Diagnosis - Severe Anemia( Microcytic Hypochromic) secondary to ? IDA ? MDS Cardiogenic pulmonary edema ( resolving) (secondary to Heart failure with preserved ejection fraction Ef-62% Renal AKI on CKD stage 3b ? .
K/c/o type 2 DM since 6 years on tablet metformin 500 mg po/od,
HTN since 8 years on tab. Metoprolol 25 mg po/od
P-
Inj. Lasix 40 mg iv bd
Tab. Ecospirin Av 78/10 mg OD HS
Tab. Clinidipine 10 mg /bd
Tab. Pantop 40 mg po/0d
Syp. Cremaffin 20 ml po/hs
Nebulisation with ipravent 12 th hourly
Budecort 12 th hourly
O supplementation to maintain spo2- >94 %
MONITOR VITALS AND INFORM SOS
BP monitoring 4 th hourly
Grbs- 7 point profile
24/2/23
ICU BED NO-2
UNIT-2
DOA-21/2/23
80 year old male came with the complaints of shortness of breath since 15 days
B/ l pedal edema and facial puffiness since 3 days
Burning micturition and decreased urine output since 2 days
S-
No fever spikes yesterday
Stools not passed
O-
Patient is conscious, coherent, cooperative
Vitals-
Temp-98.2F
PR -80 bpm
RR -22cpm
Bp-140/80 mmhg
Spo2- 98% at 1 lit of O2
Grbs- 109mg/dl
Input- 800
Output -1300
On 21/2/23
8pm- 137 mg/dl
2am-137 mg/dl
On 22/2/23
8 am - 114 mg/dl
2pm- 135 mg/dl inj. Hai 4 u given
8pm- 72 mg/dl
On 23/2/23
2 am - 125 mg/dl
8 am- 93 mg/dl inj. Hai 4 u given
2pm- 106 mg/dl inj Hai 4 u given
10 pm- 274 mg/dl
24/2/23
2am- 235 mg/dl
6 am - 69 mg/dl
CVS - S1,S2 present
No murmurs
Jvp - not raised
RS- BAE+, NVBS
P/A - soft, non tender, tympanic note present
CNS-
GCS-E4V5M6
Reflexes- Right. Left
Biceps. 2+. 2+
Triceps. 1+. 1+
Supinator. 1+. 1+
Knee. 2+. 2+
Ankle. 1+. 1+
Investigations -
Hb-7.5 g/dl
Tlc- 12800
Neu-75
Lymp-20
Pcv- 26.2
PLC- 3.6
BGT- O POSITIVE
S electrolytes-
Na- 143
K-3. 1
Cl-99
Ca2+- 1.06
B. UREA-38
S creat-1. 5
Chest xray PA view-
A-
Diagnosis - Severe Anemia( Microcytic Hypochromic) secondary to ? IDA ? MDS .Cardiogenic pulmonary edema ( resolving) (secondary to Heart failure with preserved ejection fraction Ef-62% Renal AKI on CKD stage 3b ? .
K/c/o type 2 DM since 6 years on tablet metformin 500 mg po/od,
HTN since 8 years on tab. Metoprolol 25 mg po/od
2units PRBC transfusion done
P
Inj. Lasix 40 mg iv bd
Tab. Ecospirin Av 75/20 mg OD HS
Tab. Clinidipine 10 mg /bd
Tab. Pantop 40 mg po/0d/bbf
Syp. Cremaffin 20 ml po/bd
Nebulisation with ipravent 12 th hourly
Budecort 12 th hourly
O supplementation to maintain spo2- >92%
MONITOR VITALS AND INFORM SOS
BP monitoring 4 th hourly
Grbs- 7 point profile
25/2/23
AMC BED NO-5
UNIT-2
DOA-21/2/23
80years old male came with the complaints of shortness of breath since 15 days
B/ l pedal edema and facial puffiness since 3 days
Burning micturition and decreased urine output since 2 days
S-
No fever spikes yesterday
Stools not passed
O-
Patient is conscious, coherent, cooperative
Vitals-
Temp-98.F
PR -72 bpm
RR -24 cpm
Bp-150/80 mmhg
Spo2- 98% at 1 lit of O2
Grbs- 75mg/dl
Input- 800
Output -1300
On 21/2/23
8pm- 137 mg/dl
2am-137 mg/dl
On 22/2/23
8 am - 114 mg/dl
2pm- 135 mg/dl inj. Hai 4 u given
8pm- 72 mg/dl
On 23/2/23
2 am - 125 mg/dl
8 am- 93 mg/dl inj. Hai 4 u given
2pm- 106 mg/dl inj Hai 4 u given
10 pm- 274 mg/dl
24/2/23
2am- 235 mg/dl
6 am - 69 mg/dl
8am-109mg/dl
2pm- 195 mg/dl
8pm- 103 mg/dl inj. Hai 4 units given
25/2/23
12am- 226 mg/dl
2am- 394 mg/dl
8 am- 75 mg/dl
CVS - S1,S2 present
No murmurs
Jvp - not raised
RS- BAE+, NVBS
P/A - soft, non tender, tympanic note present
CNS-
GCS-E4V5M6
Reflexes- Right. Left
Biceps. 2+. 2+
Triceps. 1+. 1+
Supinator. 1+. 1+
Knee. 2+. 2+
Ankle. 1+. 1+
Investigations -
Hb-8.1 g/dl
Tlc- 17100
Neu-74
Lymp-15
Pcv- 28.7
PLC- 4.1
BGT- O POSITIVE
S electrolytes-
Na- 137
K-3. 1
Cl-95
Ca2+- 0.96
B. UREA-37
S creat-1. 4
A-
Diagnosis - Severe Anemia( Microcytic Hypochromic) secondary to ? IDA ? MDS .Cardiogenic pulmonary edema ( resolving) (secondary to Heart failure with preserved ejection fraction Ef-62% Renal AKI on CKD stage 3b ? .
K/c/o type 2 DM since 6 years on tablet metformin 500 mg po/od,
HTN since 8 years on tab. Metoprolol 25 mg po/od
C/o sob decreased
2units PRBC transfusion done
P
Inj. Lasix 40 mg iv bd
Inj. Hai s/c tid according to grbs
Tab. Ecospirin Av 75/20 mg OD HS
Tab. Clinidipine 10 mg /bd
Tab. Pantop 40 mg po/0d/bbf
Tab. Augmentin 625 mg po/tid
Syp. Potkior 10 ml po /tid
Syp. Cremaffin 20 ml po/bd
Nebulisation with ipravent 12 th hourly
Budecort 12 th hourly
O supplementation to maintain spo2- >92%
MONITOR VITALS AND INFORM SOS
BP monitoring 4 th hourly
Grbs- 7 point profile







Comments
Post a Comment