70yr old male with altered sensorium secondary to ?Meningitis
Sri Nithya
Roll.no-86
ICU-BED. NO -03
A 70 Years Old Man Who was a Farmer By Occupation Presented to Casualty With
Altered Sensorium Since 3 Days
Fever Since 20 Days
HOPI :
Patient Was Apparently Asymptomatic Till 2014 ;
2014 - Patient Had Fever Associated with Cough for which he went to Hospital & Was Diagnosed to Have ? Pneumonia with DENOVO DM2 & Was Prescribed with OHAs ( Tab.METFORMIN & Tab.GLIMIPRIDE )
6 Months Back - Patient Had Fever Associated with Cough for Which he Went to Hospital & Said to Have High Sugars along with Lung Infection ; Got Treated & Discharged in a Hemodynamically Stable Manner.Started using insulin for Diabetes Since Then
20 Days Back : Patient Had Fever with Cough ; For Which He went to Hospital & Suspected to Have TB But Reports Turned out to be Negative & Patient Discharged as LAMA & When He Returned Home 3 Days Back He Gradually Developed Altered Sensorium & Couldn't Recognise His Attendants
Past History :
K/C/O DM2 Since 9 Years and on Regular Medications
N/K/C/O HTN ; TB ; EPILEPSY ; ASTHMA
Addictions :
He Started Consumption of Alcohol at the age of 20years & It became a habit to drink 90ml per Day Till 6 Months Back
He Started Smoking Beedis at the age of 20 Years & It Became a Habit to Smoke 20 Beedis Per Day
On Presentation :
BP - 110/80mmHg
PR - 110/min
Temp - 102.5 F
RR - 22/min
Spo2 - 98% @RA
CVS - S1S2 Heard & No Murmurs
RS - BAE + ; NVBS +
P/A - Soft & Non Tender
CNS -
GCS - E2V2M5
RT Pupil - Couldn't be assessed
Lt Pupil - NSRL
Tone - Normal in Both UL & Hypertonia in Both lower limbs
Power - 4/5 In all 4 Limbs
Reflexes - B T S K A - 2+
Plantars - RT - Mute & Left - Flexor
Investigations -
ECG-
S. Urea-24mg/dl
S creatine-0. 8mg/dl
S. Electrolytes -
Na+-132
K+- 3.6
Cl- 98
Ca2+ 1.20
LFT-
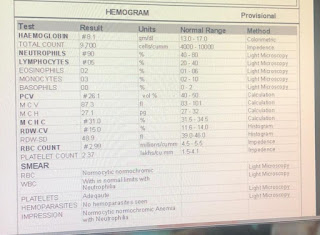
Hemogram-
Rbs-157mg/dl
HbA1c-6. 8%
ABG-
CSF analysis-
glucose -42
Protein -60
Cl-121
ADA-131
CSF CELL COUNT
Vol-0. 5 ml
Color- colorless
Appearance- clear
Total count-104 cells
DC-
60% lymphocytes
20% monocytes
20% neutrophils
Others- nil
RBC- nil
Provisional diagnosis -
?TB meningitis
Treatment -
Ryles tube feeds-200 ml milk every 4 th hourly
100 ml water every hourly
Iv fluids NS @50 ml/hr
Inj. Ceftriaxone 2 GM iv stat
Then inj . Ceftriaxone 1 GM iv bd
Inj Dexa 6 mg iv stat then
Inj. Dexa 6mg iv tid
Monitor vitals 2 nd hourly
Grbs monitoring
Strict input and output charting
Inj. Neomol 1 GM iv /sos ( if temp>101F)
16/02/23
ICU-BED NO. 3
UNIT-2
DOA-15/2/23
70 year old man c/o fever since 20 days and altered sensorium since 3 days
S-
No fever spikes
Patient obeying to commands
O-
BP - 120/70mmHg
PR - 98/min
Temp - 98F
RR - 22/min
Spo2 - 98% @RA
Grbs-250 mg/dl
CVS - S1S2 Heard & No Murmurs
RS - BAE + ; NVBS +
P/A - Soft & Non Tender
CNS -
GCS - E2V2M5
RT Pupil - Couldn't be assessed
Lt Pupil - NSRL
A-
Altered sensorium under evaluation secondary to? meningitis
?TB meningitis
Investigations -
Hb- 12.0g/dl
TLC- 8700
PLC- 3.02LAKHS
Lymphocytes -32
Pcv-35. 2
S Urea-24mg/dl
S creatine-0. 8mg/dl
S. Electrolytes -
Na+-132
K+- 3.6
Cl- 98
Ca2+ 1.20
LFT-
Total bilirubin-0. 9
ALP-144
Total proteins-6. 2
Albumin-3. 0
Rbs-157mg/dl
HbA1c- 6.8%
P-
Ryles tube feeds-200 ml milk every 4 th hourly
100 ml water every hourly
Iv fluids NS @50 ml/hr
Inj. Ceftriaxone 2 GM iv stat
Then inj . Ceftriaxone 1 GM iv bd
Inj Dexa 6 mg iv stat then
Inj. Dexa 6mg iv tid
Monitor vitals 2 nd hourly
Grbs monitoring
Strict input and output charting
Inj. Neomol 1 GM iv /sos ( if temp>101F)
Inj. HAI S/C according to grbs
17/02/23
ICU-BED NO. 3
UNIT-2
DOA-15/2/23
70 year old man c/o fever since 20 days and altered sensorium since 3 days
S-
No fever spikes
Patient obeying to commands
Hiccups since yesterday afternoon
O-
BP - 110/70mmHg
PR - 66/min
Temp - 95.5F
RR - 22/min
Spo2 - 98% @RA
Grbs-
15/2/23
8am-250mg/dl
2pm-269mg/dl
4pm-272mg/dl
8pm-278mg/dl
16/2/23
2am - 200 mg/dl
8am - 250mg /dl
2pm 265mg/dl
8pm 140mg/dl
10pm 191 mg/dl
17/2/23
2am 197 mg/dl
8am 175mg/dl
Input-2300ml
Out put-1000ml
CVS - S1S2 Heard & No Murmurs
RS - BAE + ; NVBS +
P/A - Soft & Non Tender
CNS -
GCS - E3V3M5
RT Pupil - Couldn't be assessed
Lt Pupil - NSRL
Tone- normal in all 4 limbs
Power- 4/5 in all 4 limbs
A-
Altered sensorium(resolving) secondary to meningoencephalitis secondary to tuberculosis
K/c/o DM since 9 years
Investigations -
Hb- 11.5g/dl
TLC- 11000
PLC- 3.08LAKHS
Neutrophils -85
Lymphocytes -09
Pcv 34.6
RBC count 3.08
15/2/23
S.Electrolytes -
Na-135
K-4. 3
Cl-102
Ca2+1. 12
P-
Ryles tube feeds-200 ml milk every 4 th hourly
100 ml water every hourly
Iv fluids NS @100 ml/hr
Inj. Dexa 6mg iv tid day 3
Inj human actrapid s/c according to GRBS
Tab. Isoniazid 275 mg (4tabs po/od) morning
Tab. Rifampicin 550 mg (4tabs po/od morning
Tab. Pyrazinamide 1550mg (4tabs po od morning
Tab ethambutol 825 mg po od morning
Grbs 7 th hourly
Inj. neomol 1 g iv sos( if temp >101F)
Strict input output charting
Grbs monitoring
Tab benadone 40mg po/od
Tab baclofen 10mg po/sos
Inj perinorm 10mg iv stat
Inj pan 40mg iv/od
Beautiful Orange colored urine is seen might be due to antitubercular therapy - Rifampicin
18/02/23
ICU-BED NO. 3
UNIT-2
DOA-15/2/23
70 year old man c/o fever since 20 days and altered sensorium since 3 days
S-
C/o hiccups since 3 days
Sensorium - increased drowsiness
O-
BP - 130/80mmHg
PR - 80/min
Temp - 98.2F
RR - 20/min
Spo2 - 98% @RA
Grbs-
15/2/23
8am-250mg/dl
2pm-269mg/dl
4pm-272mg/dl
8pm-278mg/dl
16/2/23
2am - 200 mg/dl
8am - 250mg /dl
2pm 265mg/dl
8pm 140mg/dl
10pm 191 mg/dl
17/2/23
2am 197 mg/dl
8am 175mg/dl
4pm-92mg/dl 6u HAI given
8pm- 125 mg/dl
18/02/23
2am- 168mg/dl
8am-101 mg/dl 4 units HAI given
Input-2800ml
Out put-2400ml
CVS - S1S2 Heard & No Murmurs
RS - BAE + ; NVBS +
P/A - Soft & Non Tender
CNS - patient is drowsy not oriented to time, place and person
GCS - E2V3M5
RT Pupil - Couldn't be assessed
Lt Pupil - NSRL
Tone- normal in all 4 limbs
Power- 4/5 in all 4 limbs
Reflexes-
Right. Left
Biceps. 2+. 2+
Triceps. 2+. 2+
Supinator. 1+. 2+
Knee. 2+. 2+
Ankle. 1+. 1+
Plantar. Decreased. Decreased
Investigations -
Hb- 11.6g/dl
TLC- 9300
PLC- 3.19LAKHS
Neutrophils -77
Lymphocytes -16
Pcv -34.9
RBC count 3.71
18/2/23
S.Electrolytes -
Na-124
K-3. 8
Cl-99
Ca2+-1.20
A-
Altered sensorium(resolving) secondary to meningoencephalitis secondary to tuberculosis
K/c/o DM since 9 years
P-
Ryles tube feeds-200 ml milk every 4 th hourly
100 ml water every hourly
Iv fluids NS @100 ml/hr
Inj. Dexa 6mg iv tid day 3
Inj human actrapid s/c according to GRBS
Inj. Pan 40 mg iv od
Inj . NEOMOL 1g iv /sos if temp >101F
Tab. Isoniazid 275 mg (4tabs po/od) morning
Tab. Rifampicin 550 mg (4tabs po/od morning
Tab. Pyrazinamide 1550mg (4tabs po od morning
Tab ethambutol 825 mg po od morning
Tab. Benadone 40 mg po/od
Tab. Baclofen 10 mg po/sos
Grbs 7 th hourly
Strict input output charting
19/02/23
ICU-BED NO. 3
UNIT-2
DOA-15/2/23
70 year old man c/o fever since 20 days and altered sensorium since 3 days
S-
Fever spike at 7am
Patient obeying to commands
Hiccups since 4 days
O-
Patient is drowsy not oriented to place time and person
BP - 110/80mmHg
PR - 106/min
Temp - 98.2F
RR - 22/min
Spo2 - 96% @RA
GRBS 140mg/dl
18/2/23
8am 101
4pm 208
8pm 219
Grbs-
15/2/23
8am-250mg/dl
2pm-269mg/dl
4pm-272mg/dl
8pm-278mg/dl
16/2/23
2am - 200 mg/dl
8am - 250mg /dl
2pm 265mg/dl
8pm 140mg/dl
10pm 191 mg/dl
17/2/23
2am 197 mg/dl
8am 175mg/dl
Input-3000ml
Out put-3400ml
CVS - S1S2 Heard & No Murmurs
RS - BAE + ; NVBS +
P/A - Soft & Non Tender
CNS -
GCS - E3V3M5
RT Pupil - Couldn't be assessed
Lt Pupil - NSRL
Tone- normal in all 4 limbs
Power- 4/5 in all 4 limbs
A-
Altered sensorium(resolving) secondary to meningoencephalitis secondary to tuberculosis
K/c/o DM since 9 years
Investigations -
Hb- 12.9g/dl
TLC- 13100
PLC- 3.11
Neutrophils -80
Lymphocytes -14
Pcv 38.7
Mcv 39.3
RBC count 4.15
Sodium 137
Potassium 3.8
Chloride 97
Ionized calcium 1.1
15/2/23
S.Electrolytes -
Na-135
K-4. 3
Cl-102
Ca2+1. 12
P-
Ryles tube feeds-200 ml milk every 4 th hourly
100 ml water every hourly
Iv fluids NS @100 ml/hr
Inj. Dexa 6mg iv tid day 5
Inj human actrapid s/c according to GRBS
Tab. Isoniazid 275 mg (4tabs po/od) morning
Tab. Rifampicin 550 mg (4tabs po/od morning
Tab. Pyrazinamide 1550mg (4tabs po od morning
Tab ethambutol 825 mg po od morning
Grbs 7 th hourly
Inj. neomol 1 g iv sos( if temp >101F)
Strict input output charting
Grbs monitoring
Tab baclofen 10mg po/sos
Inj pan 40mg iv/od
ECG-
19/02/23
ICU-BED NO. 3
UNIT-2
DOA-15/2/23
70 year old man c/o fever since 20 days and altered sensorium since 3 days
S-
Fever spike at 11pm, 7am, 11 am
Hiccups subsided
O-
Patient is drowsy not oriented to place time and person responding to only deep pain stimulation
BP - 90/60mmHg
PR - 68/min
Temp - 98.2F
RR - 24/min
Spo2 - 90 % @RA
99%on 2l o2
GRBS 161mg/dl
Input-3000ml
Out put-3400ml
CVS - S1S2 Heard & No Murmurs
RS - BAE + ; NVBS +
P/A - Soft & Non Tender
CNS -
GCS - E2V1M3
RT Pupil - Couldn't be assessed
Lt Pupil - decreased size , non reactive to light
Tone- normal on right side
Decreased on left side
Dolls eye positive bilateral
Jaw jerk absent
Right. Left
Biceps 2+. -
Triceps. 2+. -
Supinator. 1+. -
Knee 2+. -
ankle 1+. -
Plantars bilateral mute
A-
Altered sensorium secondary to meningoencephalitis secondary to tuberculosis
K/c/o DM since 9 years
With ? Old pulmonary kochs
Acute infarct in ? PCA? MCA territory
With new onset left hemiplegia
P-
Ryles tube feeds-200 ml milk every 4 th hourly
100 ml water every hourly
Iv fluids NS @100 ml/hr
Inj. Dexa 6mg iv tid day 5
Inj human actrapid s/c according to GRBS
Tab baclofen 10mg po/sos
Inj pan 40mg iv/od
Tab. Isoniazid 275 mg (4tabs po/od) morning
Tab. Rifampicin 550 mg (4tabs po/od morning
Tab. Pyrazinamide 1550mg (4tabs po od morning
Tab ethambutol 825 mg po od morning
Grbs 7 th hourly
Inj. neomol 1 g iv sos( if temp >101F)
Strict input output charting
Grbs monitoring
Chest xray -
Sr . electrolytes
Na-138
K-3. 8
Cl-99
Ca2+- 1.20
MRI images
20/02/23
ICU-BED NO. 3
UNIT-2
DOA-15/2/23
70 year old man c/o fever since 20 days and altered sensorium since 3 days
S-
Fever spike at 2 am 100. 4F
Hiccups subsided
O-
Patient is drowsy not oriented to place time and person responding to only deep pain stimulation
BP - 110/70mmHg
PR - 86/min
Temp - 98.6F
RR - 22/min
Spo2 - 97 % @RA
GRBS 119mg/dl
Input-3400ml
Out put-1900ml
CVS - S1S2 Heard & No Murmurs
RS - BAE + ; NVBS +
P/A - Soft & Non Tender
CNS -
GCS - E2V1M4
RT Pupil - Couldn't be assessed
Lt Pupil - dilated , sluggishly reacting to light
Tone- normal on right side
Decreased on left side
Dolls eye positive bilateral
Jaw jerk absent
Right. Left
Biceps 2+. 2 +
Triceps. 2+. 1+
Supinator. 1+. 1+
Knee 2+. 1+
ankle 1+. -
Plantars bilateral flexors
Power- right. Left
UL. 3/5. 0/5
LL. 3/5. 2/5
INVESTIGATIONS -
Hb-12. 1g/dl
B urea -41 mg/dl
S creat -0. 7 mg/dl
S electrolytes-
Na-136
K-3. 7
Cl-98
Ca2+1.21
19/02/23
Ph-7. 48
Pco2-31. 8
Po2-75. 7
Hco3-23. 9
Na-126
K-3. 6
Ca2-0. 92
Cl-99
20/2/23-
Ph-7. 42
Pco2-30. 4
Po2-78. 5
Hco3-19. 7
Na-124
K-2. 9
Ca2-0. 52
Cl-96
A-
Altered sensorium secondary to meningoencephalitis secondary to tuberculosis
K/c/o DM since 9 years
With ? Old pulmonary kochs
Acute infarct in ? PCA? MCA territory
With new onset left hemiplegia
P-
Ryles tube feeds-200 ml milk every 4 th hourly
100 ml water every hourly
Iv fluids NS @100 ml/hr
Inj. Dexa 6mg iv tid day 5
Inj human actrapid s/c according to GRBS
Inj. neomol 1 g iv sos( if temp >101F)
Inj pan 40mg iv/od
Tab baclofen 10mg po/sos
Tab. Isoniazid 275 mg (4tabs po/od) morning
Tab. Rifampicin 550 mg (4tabs po/od morning
Tab. Pyrazinamide 1550mg (4tabs po od morning
Tab ethambutol 825 mg po od morning
Tab. Pyridoxine 40 mg RT/OD
Tab. Ecospirin 150 mg RT/OD
Tab. Clopidogrel 75mg RT/OD
Tab. Atorvastatin 20 mgRT/OD HS
Frequent changes in position
Grbs 7 point profile
Strict input output charting
Grbs monitoring
21/02/23
ICU-BED NO. 3
UNIT-2
DOA-15/2/23
70 year old man c/o fever since 20 days and altered sensorium since 3 days
S-
2 fever spikes one at
9pm yesterday night 101F
7am 101.4F
Stools not passed
Hiccups subsided
O-
Patient is drowsy ,not arousable, not oriented to place time and person
Febrile on touch
BP - 120/80mmHg
PR - 82/min
Temp - 101.2F
RR - 24/min
Spo2 - 95% @RA
GRBS 164mg/dl
Input-2400ml
Out put-2000ml
CVS - S1S2 Heard & No Murmurs
RS - BAE + ; NVBS +
P/A - Soft & Non Tender
CNS -
GCS - E1V1M5
RT Pupil - Couldn't be assessed
Lt Pupil - normal in size not reacting to light
Tone- normal on right side
Decreased on left side
Dolls eye positive bilateral
Jaw jerk absent
Right. Left
Biceps 2+. 2 +
Triceps. 2+. 1+
Supinator. 1+. -
Knee 1+. -
ankle -. -
Plantars bilateral flexors
Power- right. Left
UL. 3/5. 0/5
LL. 2/5. 1/5
INVESTIGATIONS -
Hb-14.6g/dl
TLC 9300
Neu 71
Lymp 21
Plc 3.17
Pcv 40.8
B urea-29 mg/dl
S creat-0. 6 mg/dl
S electrolytes-
Na-136
K-3. 9
Cl-99
Ca2+1.09
Lft
Tb 1.45
Db 0.21
Alp 247
Total protein 5.5
Albumin 2.44
19/02/23
Ph-7. 48
Pco2-31. 8
Po2-75. 7
Hco3-23. 9
Na-126
K-3. 6
Ca2-0. 92
Cl-99
20/2/23-
Ph-7. 42
Pco2-30. 4
Po2-78. 5
Hco3-19. 7
Na-124
K-2. 9
Ca2-0. 52
Cl-96
A-
Altered sensorium secondary to meningoencephalitis secondary to tuberculosis (on ATT since 15/2/23) with ?old pulmonary kochs with acute infarct in right thalamus and striati capsular region ,left midbrain, cerebellar hemisphere
K/c/o DM since 9 years
With left hemiplegia (new onset)
With ? Old pulmonary kochs
Acute infarct in ? PCA? MCA territory
With new onset left hemiplegia
P-
Ryles tube feeds-200 ml milk every 4 th hourly
100 ml water every hourly
Iv fluids NS @100 ml/hr
Inj. Dexa 6mg iv tid day 7
Inj HAI s/c according to GRBS
Inj. neomol 1 g iv sos( if temp >101F)
Inj pan 40mg iv/od
Tab baclofen 10mg po/sos
Tab. Isoniazid 275 mg (4tabs po/od) morning
Tab. Rifampicin 550 mg (4tabs po/od morning
Tab. Pyrazinamide 1550mg (4tabs po od morning
Tab ethambutol 825 mg po od morning
Tab. Pyridoxine 40 mg RT/OD
Tab. Ecospirin 150 mg RT/OD
Tab. Clopidogrel 75mg RT/OD
Tab. Atorvastatin 20 mgRT/OD HS
Tab. Baclofen 10 mg RT/OD sos
Frequent changes in position
Grbs 7 th hourly
Left upper limb and lower limb and chest physiotherapy twice daily
Sir bed and position change 2nd hourly
Eyecare
Oral suctioning 4th hourly
Strict input output charting
Grbs monitoring
22/02/23
ICU-BED NO. 3
UNIT-2
DOA-15/2/23
70 year old man c/o fever since 20 days and altered sensorium since 3 days
S-
Fever spikes present
7am 101.9F
Stools not passed
Hiccups subsided
O-
Patient is drowsy ,not arousable
Febrile on touch
BP - 130/80mmHg
PR - 102/min
Temp - 102.2F
Spo2 - 88% @RA
And 100 percent on 2 lit of O2
GRBS 194mg/dl
Input 2000ml
Out put-1400ml
CVS - S1S2 Heard & No Murmurs
RS - BAE + ; NVBS +
P/A - Soft & Non Tender
CNS -
GCS - E1V1M5
RT Pupil - Couldn't be assessed
Lt Pupil - normal in size
Sluggishly reacting to light
Tone- normal on right side
Decreased on left side
Right. Left
Biceps 2+. 1 +
Triceps. 1+. 1+
Supinator. -. -
Knee 2+. 1+
ankle 1+ -
Plantars bilateral flexors
Power- right. Left
UL. 3/5. 0/5
LL. 2/5. 0/5
INVESTIGATIONS -
22/2/23
Na-131
K-3. 8
Cl-97
Ca2+1.10
Hb-14.6g/dl
TLC 9300
Neu 71
Lymp 21
Plc 3.17
Pcv 40.8
B urea-29 mg/dl
S creat-0. 6 mg/dl
S electrolytes-
Na-136
K-3. 9
Cl-99
Ca2+1.09
Lft
Tb 1.45
Db 0.21
Alp 247
Total protein 5.5
Albumin 2.44
19/02/23
Ph-7. 48
Pco2-31. 8
Po2-75. 7
Hco3-23. 9
Na-126
K-3. 6
Ca2-0. 92
Cl-99
20/2/23-
Ph-7. 42
Pco2-30. 4
Po2-78. 5
Hco3-19. 7
Na-124
K-2. 9
Ca2-0. 52
Cl-96
A-
Altered sensorium secondary to meningoencephalitis secondary to tuberculosis (on ATT since 15/2/23) with ?old pulmonary kochs with acute infarct in right thalamus and striati capsular region ,left midbrain, cerebellar hemisphere
K/c/o DM since 9 years
With left hemiplegia (new onset)
With ? Old pulmonary kochs
Acute infarct in ? PCA? MCA territory
With new onset left hemiplegia
P-
Ryles tube feeds-200 ml milk every 4 th hourly
200 ml water every hourly
Iv fluids NS @100 ml/hr
Inj. Dexa 6mg iv tid day 8
Inj HAI s/c according to GRBS
Inj. neomol 1 g iv sos( if temp >101F)
Inj pan 40mg iv/od
Tab baclofen 10mg po/sos
Tab. Isoniazid 275 mg (4tabs po/od) morning
Tab. Rifampicin 550 mg (4tabs po/od morning
Tab. Pyrazinamide 1550mg (4tabs po od morning
Tab ethambutol 825 mg po od morning
Tab. Pyridoxine 40 mg RT/OD
Tab. Ecospirin 150 mg RT/OD
Tab. Clopidogrel 75mg RT/OD
Tab. Atorvastatin 20 mgRT/OD HS
Tab. Baclofen 10 mg RT/OD sos
Nebulization with mucomist 6th hourly
Frequent changes in position
Grbs 7 th hourly
Left upper limb and lower limb and chest physiotherapy twice daily
Sir bed and position change 2nd hourly
Eyecare
Oral suctioning 4th hourly
Strict input output charting
Grbs monitoring
Syp cremaffin plus 30ml po/hs
23/02/23
ICU-BED NO. 3
UNIT-2
DOA-15/2/23
70 year old man c/o fever since 20 days and altered sensorium since 3 days
S-
Fever spikes present
Stools passed yesterday after enema
Hiccups subsided
Developed bed sore
O-
Patient is drowsy ,not arousable
Febrile on touch
BP - 110/70mmHg
PR - 111/min
Temp - 99.4F
Spo2 -100 percent on 2 lit of O2
GRBS 183mg/dl
Inj hai given 6 units
Input 1150ml
Out put-1050ml
CVS - S1S2 Heard & No Murmurs
RS - BAE + ; crepts present in right IAA,ISA,MA
P/A - Soft & Non Tender
CNS -
GCS - E1V1M4
RT Pupil - Couldn't be assessed
Lt Pupil - normal in size
Sluggishly reacting to light
Tone- normal on right side
Decreased on left side
Right. Left
Biceps 1+. 1 +
Triceps. 1+. 1+
Supinator. -. -
Knee 1+. 1+
ankle - -
Plantars bilateral flexors
Power- right. Left
UL. 3/5. 0/5
LL. 2/5. 0/5
INVESTIGATIONS -
23/2/23
Hb 11.6
TLC 11900
N 78
L 20
Pcv 35.6
Plt 3.2
S.creat 0.7
Blood urea 31
Na 139
K 3.7
Cl 98
Calcium 1.10
22/2/23
Na-131
K-3. 8
Cl-97
Ca2+1.10
Hb-14.6g/dl
TLC 9300
Neu 71
Lymp 21
Plc 3.17
Pcv 40.8
B urea-29 mg/dl
S creat-0. 6 mg/dl
S electrolytes-
Na-136
K-3. 9
Cl-99
Ca2+1.09
Lft
Tb 1.45
Db 0.21
Alp 247
Total protein 5.5
Albumin 2.44
19/02/23
Ph-7. 48
Pco2-31. 8
Po2-75. 7
Hco3-23. 9
Na-126
K-3. 6
Ca2-0. 92
Cl-99
20/2/23-
Ph-7. 42
Pco2-30. 4
Po2-78. 5
Hco3-19. 7
Na-124
K-2. 9
Ca2-0. 52
Cl-96
A-
Altered sensorium secondary to meningitis secondary to tuberculosis (on ATT since 15/2/23) with ?old pulmonary kochs with acute infarct in right thalamus and striati capsular region ,left midbrain, cerebellar hemisphere
K/c/o DM since 9 years
With left hemiplegia (new onset)
With ? Old pulmonary kochs
Acute infarct in ? PCA? MCA territory
With new onset left hemiplegia
P-
Ryles tube feeds-200 ml milk every 4 th hourly
200 ml water every hourly
Iv fluids NS @100 ml/hr
Inj. Dexa 6mg iv tid day 9
Inj monocef 1gm iv/bd day 2
Inj HAI s/c according to GRBS
Inj. neomol 1 g iv sos( if temp >101F)
Inj pan 40mg iv/od
Tab baclofen 10mg po/sos
Tab. Isoniazid 275 mg (4tabs po/od) morning
Tab. Rifampicin 550 mg (4tabs po/od morning
Tab. Pyrazinamide 1550mg (4tabs po od morning
Tab ethambutol 825 mg po od morning
Tab. Pyridoxine 40 mg RT/OD
Tab. Ecospirin 150 mg RT/OD
Tab. Clopidogrel 75mg RT/OD
Tab. Atorvastatin 20 mgRT/OD HS
Nebulization with mucomist 6th hourly
Frequent changes in position
Grbs 7 th hourly
Left upper limb and lower limb and chest physiotherapy twice daily
Air bed and position change 2nd hourly
Eyecare
Oral suctioning 4th hourly
Strict input output charting
Syp cremaffin plus 30ml po/hs
Protein X powder 2tbs in 1 glass of milk iv/tid
24/02/23
ICU-BED NO. 3
UNIT-2
DOA-15/2/23
70 year old man c/o fever since 20 days and altered sensorium since 3 days
S-
Fever spikes present
Stools passed yesterday
Hiccups subsided
Developed bed sore
O-
Patient is drowsy ,not arousable with deep pain stimulation
Febrile on touch
BP - 100/60mmHg
PR - 112/min
Temp - 100.2F
Spo2 -98 percent on 2 lit of O2
RR. 26cpm
GRBS 141mg/dl
Inj hai given 4 units
Input 2000ml
Out put-1300ml
CVS - S1S2 Heard & No Murmurs
RS - BAE + ; crepts present in right IAA,ISA,MA
P/A - Soft & Non Tender
CNS -
GCS - E1V2M4
RT Pupil - Couldn't be assessed
Lt Pupil - dilated
Sluggishly reacting to light
Right. Left
Biceps 2+. 1 +
Triceps. 2+. 1+
Supinator. 1+ 1+
Knee 2+. 2+
ankle 1+. 1+
Plantars bilateral flexors
Power- right. Left
UL. 3/5. 0/5
LL. 2/5. 0/5
INVESTIGATIONS -
24/2/23
Hb 11.3
Tc 16100
N 84
L 12
Pcv 34.0
RBC 3.6
Plt 3.1
Blood urea 30
Serum creatinine 0.6
Sodium 138
Potassium 3.7
Calcium 1.02
Chloride 99
Csf analysis
Sugars 73
Protein 40
Chloride 105
CSF
Volume 1 ml
Appearance clear
Color colourless
Tc 7 cells
Dc 100% L
RBC nil
23/2/23
Hb 11.6
TLC 11900
N 78
L 20
Pcv 35.6
Plt 3.2
S.creat 0.7
Blood urea 31
Na 139
K 3.7
Cl 98
Calcium 1.10
22/2/23
Na-131
K-3. 8
Cl-97
Ca2+1.10
Hb-14.6g/dl
TLC 9300
Neu 71
Lymp 21
Plc 3.17
Pcv 40.8
B urea-29 mg/dl
S creat-0. 6 mg/dl
S electrolytes-
Na-136
K-3. 9
Cl-99
Ca2+1.09
Lft
Tb 1.45
Db 0.21
Alp 247
Total protein 5.5
Albumin 2.44
19/02/23
Ph-7. 48
Pco2-31. 8
Po2-75. 7
Hco3-23. 9
Na-126
K-3. 6
Ca2-0. 92
Cl-99
20/2/23-
Ph-7. 42
Pco2-30. 4
Po2-78. 5
Hco3-19. 7
Na-124
K-2. 9
Ca2-0. 52
Cl-96
A-
TB meningitis with vasculitis
Altered sensorium secondary to acute meningitis
acute infarct in right thalamus and striati capsular region ,left midbrain, cerebellar hemisphere with ? old pulmonary kochs (on ATT since 15/2/23 started clinically)
K/c/o DM since 9 years
P-
Ryles tube feeds-200 ml milk every 4 th hourly
200 ml water every hourly
Iv fluids NS @100 ml/hr
Inj. Dexa 8mg iv tid day 10
Inj monocef 1gm iv/bd day 3
Inj HAI s/c according to GRBS
Inj. neomol 1 g iv sos( if temp >101F)
Inj pan 40mg iv/od
Tab. Isoniazid 275 mg (4tabs po/od) morning
Tab. Rifampicin 550 mg (4tabs po/od morning
Tab. Pyrazinamide 1550mg (4tabs po od morning
Tab ethambutol 825 mg po od morning
Tab. Pyridoxine 40 mg RT/OD
Tab. Ecospirin 150 mg RT/OD
Tab. Clopidogrel 75mg RT/OD
Tab. Atorvastatin 20 mgRT/OD HS
Nebulization with mucomist 6th hourly
Syp cremaffin plus 30ml po/hs
Protein X powder 2tbs in 1 glass of milk iv/tid
Grbs 7 th hourly
Left upper limb and lower limb and chest physiotherapy twice daily
Air bed and position change 2nd hourly
Eyecare
Oral suctioning 4th hourly
Strict input output charting
25/02/23
ICU-BED NO. 3
UNIT-2
DOA-15/2/23
70 year old man c/o fever since 20 days and altered sensorium since 3 days
S-
Fever spikes present
Stools not passed
Hiccups subsided
Developed bed sore
O-
Patient is drowsy ,not arousable with deep pain stimulation
BP - 110/70mmHg
PR - 106/min
Temp - 98.2F
Spo2 -93 on room air
RR. 26cpm
GRBS 179mg/dl
Inj hai given 6 units
Input 2600ml
Out put-1500ml
CVS - S1S2 Heard & No Murmurs
RS - BAE + ; NVBS+
P/A - Soft & Non Tender
CNS -
GCS - E2V2M4
RT Pupil - Couldn't be assessed
Lt Pupil - small sized pupil
Sluggishly reacting to light
Right. Left
Biceps 2+. 1 +
Triceps. 2+. 1+
Supinator. 1+ 1+
Knee 2+. 2+
ankle 1+. 1+
Plantars bilateral flexors
Power- right. Left
UL. 3/5. 0/5
LL. 2/5. 0/5
INVESTIGATIONS -
25/2/23
Hb 10.4
Tc 14300
N 83
L 12
Pcv 31.1
Plt 2.29
S creat 1.4
Na 140
K 3.7
Cl 98
Calcium ionised 1.04
CSF Ada 09
CSF chloride 105
24/2/23
Hb 11.3
Tc 16100
N 84
L 12
Pcv 34.0
RBC 3.6
Plt 3.1
Blood urea 30
Serum creatinine 0.6
Sodium 138
Potassium 3.7
Calcium 1.02
Chloride 99
Csf analysis
Sugars 73
Protein 40
Chloride 105
CSF
Volume 1 ml
Appearance clear
Color colourless
Tc 7 cells
Dc 100% L
RBC nil
23/2/23
Hb 11.6
TLC 11900
N 78
L 20
Pcv 35.6
Plt 3.2
S.creat 0.7
Blood urea 31
Na 139
K 3.7
Cl 98
Calcium 1.10
22/2/23
Na-131
K-3. 8
Cl-97
Ca2+1.10
Hb-14.6g/dl
TLC 9300
Neu 71
Lymp 21
Plc 3.17
Pcv 40.8
B urea-29 mg/dl
S creat-0. 6 mg/dl
S electrolytes-
Na-136
K-3. 9
Cl-99
Ca2+1.09
Lft
Tb 1.45
Db 0.21
Alp 247
Total protein 5.5
Albumin 2.44
19/02/23
Ph-7. 48
Pco2-31. 8
Po2-75. 7
Hco3-23. 9
Na-126
K-3. 6
Ca2-0. 92
Cl-99
20/2/23-
Ph-7. 42
Pco2-30. 4
Po2-78. 5
Hco3-19. 7
Na-124
K-2. 9
Ca2-0. 52
Cl-96
A-
TB meningitis with vasculitis
Altered sensorium secondary to acute meningitis
acute infarct in right thalamus and striati capsular region ,left midbrain, cerebellar hemisphere with ? old pulmonary kochs (on ATT since 15/2/23 started clinically)
K/c/o DM since 9 years
P-
Ryles tube feeds-200 ml milk every 4 th hourly
200 ml water every 2nd hourly
Iv fluids NS @100 ml/hr
Inj. Dexa 16 mg iv tid day 11
Inj monocef 1gm iv/bd day 4
Inj pan 40mg iv/od
Inj heparin 5000IU sc/bd
Tab dolo 650mg po/qid
Inj HAI s/c according to GRBS
Tab. Isoniazid 275 mg (4tabs po/od) morning day 11
Tab. Rifampicin 550 mg (4tabs po/od morning day 11
Tab. Pyrazinamide 1550mg (4tabs po od morning day 11
Tab ethambutol 825 mg po od morning day 11
Tab. Pyridoxine 40 mg RT/OD
Tab. Ecospirin 150 mg RT/OD
Tab. Clopidogrel 75mg RT/OD
Tab. Atorvastatin 20 mgRT/OD HS
Nebulization with mucomist 6th hourly
Syp cremaffin plus 30ml po/hs
Protein X powder 2tbs in 1 glass of milk iv/tid
Grbs 7 th hourly
Left upper limb and lower limb and chest physiotherapy twice daily
Air bed and position change 2nd hourly
Eyecare lubrex eye drops
Night lip tapping
Oral suctioning 4th hourly
Strict input output charting
Ambulate the patient


















Comments
Post a Comment