65 year old female with complaints of involuntary movements of left upper limb since 1 day, cough since 4 days
M. Sri Nithya
Roll. No -86
Unit-2
Chief compliants
A 65 yr old female patient came to casualty with complaints of involuntary movements of Lt upper limb since 1 day
Cough since 4 days
HOPI
Pt was apparently asymptomatic 1 week ago then she developed generalised weakness , fell down from bed and complaints of pain in the hip
Involuntary movements of lt upper limb since 1 day to and fro
No history of speech abnormalities , weakness in the upper limb and lower limb .
No H/o memory loss and abnormal posturing .
Complaints of cough since 4 days ,it is productive scanty sputum - white to yellow ,non blood stained and non foul smelling
H/o inadequate controls of sugars from 4 months
N/H/o vomiting ,sob,loose stools ,pain abdomen
K/c/o type 2 DM since 30 yrs on infusion since 10 yrs
( Insulin - lispro 20-x-20 )
K/c/o HTN from 20 yrs on T prolomet - xl 50 mg
T. Atenolol 25 mg po/ od at 10 am
K/c/o hypothyroidism from 15 yrs on thyronorm 75 mcg
Previous treatment history
Hospitalised 1 yr ago for UTI
https://rishikoundinya.blogspot.com/2022/08/54-year-old-female-with-uncontrolled.html?m=1
H/o hysterectomy 30 yrs ago
Personal history
DIET- mixed
Appetite: Normal
Bowel and bladder movements are regular
Sleep: adequate
No allergies
Chews tobacco
Chews betel nut and betel leaf twice daily
General examination
Pt is conscious , incoherent, cooperative
Pallor present
No Icterus Cyanosis Clubing Lymphadenopathy
Edema present B/L pitting type extending up to knee
Vitals
BP 110/70mmhg
PR 76 BPM
RR 18 cpm
Spo2 98
Grbs. 315 mg/ dl
Systemic examination
Respiratory examination
BAE +ve and normal vesicular breath sound heard
No crepts heard
CVS examination
S1S2 heard
No murmurs heard
Abdomen examination
Soft non tender
No hepatomegaly and splenomegaly
CNS examination
Higher mental functions intact
Conscious , coherent non cooperative
Speech normal
Motor system Rt. Lt
Tone. Upper limb N. N
Lower limb. N. N
Power Upper limb N. N
Lower limb. N. N
Reflexes B. T. S. K. A
Rt. 1+1+ _1+ _
Lt. 1+1+ _1+_
Plantars. B/L flexors
No cerebellar and meningial signs
Referred to DVL department in view of dry scaly brown lesions
Patient Complaints of dry skin since 2 months
Itchy skin lesions on bilateral lower limb since 2 months
H/o application of Betnouite cream for 4 days ( 2 days back)
lesions got subsided on anterior part of bilateral lower limb.
H/o applicatibe of glyserin and other moisturizers
H/o scratching present
No H/o fever, blisters
On examination
Multiple Hyperpigmented polysized Plaques with saling noted over left foot on dorsum excoriations noted over left anterior leg
Xerosis noted over bilateral legs
Diagnosis: senile xerosis
Provisional diagnosis
Hyperglycemia with hemiballismus K/C/o type 2 DM with HTN since 20 yrs
K/c/o hypothyroidism since 15 yrs
K/c/o CKD since 2 yrs
Diabetic nephropathy with recurrent UTI with iron deficiency anemia
Investigations
Sputum sample for culture and sensitivity,gram stain and acid fast stain
Usg abdomen
B/l grade 1-2 RPD changes with raised echogenecity
Lab investigation
X ray pa view
On 13/2/23
At 12 30 am
On 14/2/23
Ecg
On 7/2/23
Fever chart
Head end elevation
Inj. Augmentin 1.2g/ iv / bd
T. Thyronorm 75 mcg po/od
T. Promet-xl 50 mg po/bd
T. Tetrabenazine 125 mg po/tid
Inj. HAI s/c tid
8am- 8 units
1pm- 8 units
8pm- 8 units
Liquid paraffin for l/a bd
T. Teczine 5 mg po / sos
Nebulisation with duolin -6th hourly budecort -12 th hourly
Inj. Lasix 40 mg iv/bd
IVF- NS@80 ml /hr
Grbs monitoring
Input and output monitoring
ON 13/2/23
Patient was diagnosed with hospital acquired pneumonia with type 1 respiratory failure with hyperglycemia (resolved) with chorea(resolved) with diabetic nephropathy with recurrent UTI with iron deficiency anemia
Patient complaints of cough since 15 days
Breathless since 10 days
And fever since 5 days
Cough is productive in nature mucoid and non blood stained more at nights and aggravated on supine position
Breathless grade 2 MMRC increased on excretion and relieved on rest
No positional variation
Not associated with wheeze
Fever is low grade not associated with chills nd rigor
Respiratory examination
Bilateral air entry present
Crepts present at bilateral infrascapular region (left>right)
Interscapular region
Left infraaxillary area
They advised
Syp ascoryl LS 2 tsp PO TID
Neb with mucomist BD
They want to plan for bronchoscopy once the patient is stable
14/02/23
ICU-BED NO. 2
UNIT 2
70 yrs old Female came with c/o generalised weakness since 1 week,
Involuntary movements of left upper limb since 1 week, cought with expectoration since 1 week
S
C/O COUGH WITH EXPECTORANTION DECREASED
STOOLS PASSED
NO FEVER SPIKES SINCE YESTERDAY NIGHT
O
PT IS C/C/C
TEMP-AFEBRILE
PR-78Bpm
SPO2-99% WITH 2L OF O2
BP-120/60mmhg
Grbs-
8 am -170 mg/dl
8 units hai given
1pm - 132 mg/dl given 6 units hai
O/E-
SYSTEMIC EXAMINATION -
CVS-S1, S2 PRESENT
NO MURMURS
RS-BAE+, crepts + in left infrascapular ,infra axillary areas
CNS- No focal Neurological deficit
P/A - Soft ,Nontender
Investigations
S. Creatine-2. 7
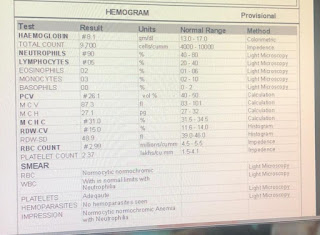
Hb-8. 1
TLC -23400
Neutrophils -81
Lymphocytes -09
Pcv-25. 4
Mcv-59. 3
Mch- 18.5
Mchc-31. 3
Rdw-16. 9
Platelet-2. 86
Na-134
K-
4.2
Cl-102
Ca2+-1.08
Blood urea-103
A-
70 yrs old Female with HOSPITAL ACQUIRED PNEUMONIA WITH TYPE 1RESPIRATORY FAILURE
WITH HYPERGLYCEMIA RESOLVED WITH CHOREA RESOLVED WITH DIABETIC NEPHROPATHY WITH REFURRENT UTI WITH IRON DEFICIENCY ANEMIA
K/C/O DM2 SINCE 30 YRS
K/C/I HYPOTHYROIDISM SINCE 15 YRS.
K/C/O CKD SINCE 2 YRS
P-
Head end elevation
Inj. Augmentin 1.2g/ iv / bd
T. Thyronorm 75 mcg po/od
T. Promet-xl 50 mg po/bd
T. Tetrabenazine 12.5 mg po/tid
Inj. HAI s/c tid
8am- 8 units
1pm- 8 units
8pm- 8 units
Liquid paraffin for l/a bd
T. Teczine 5 mg po / sos
Nebulisation with budecort -12 th hourly
Mucomist -10 th hourly
Inj. Lasix 20 mg iv/bd
IVF- NS@50 ml /hr
Grbs monitoring
Input and output monitoring
15/02/23
ICU-BED NO. 2
UNIT 2
70 yrs old Female came with c/o generalised weakness since 1 week,
Involuntary movements of left upper limb since 1 week, cought with expectoration since 1 week
S
C/O COUGH WITH EXPECTORANTION DECREASED
STOOLS PASSED YESTERDAY
NO FEVER SPIKES SINCE YESTERDAY NIGHT
O
PT IS C/C/C
TEMP-AFEBRILE
PR-78Bpm
SPO2-99% WITH 2L OF O2
BP-120/60mmhg
Grbs-
8 am -231 mg/dl
10 units hai given
O/E-
SYSTEMIC EXAMINATION -
CVS-S1, S2 PRESENT
NO MURMURS
RS-BAE+, crepts + in left infrascapular ,infra axillary areas
CNS- No focal Neurological deficit
P/A - Soft ,Nontender
Investigations -
S. Creatine-2. 8
Hb-7.8
TLC -15200
Neutrophils -75
Lymphocytes -12
Pcv-24.8
Mcv-58.9
Mch- 18.5
Mchc-31. 3
Rdw-16. 6
Platelet-2. 81
Na-134
K-3.8
Cl-102
Ca2+-1.11
Blood urea-102
A-
70 yrs old Female with HOSPITAL ACQUIRED PNEUMONIA WITH TYPE 1RESPIRATORY FAILURE( resolving)
WITH HYPERGLYCEMIA( RESOLVED )WITH CHOREA (RESOLVED) WITH DIABETIC NEPHROPATHY WITH REFURRENT UTI WITH IRON DEFICIENCY ANEMIA
K/C/O DM2 SINCE 30 YRS
K/C/I HYPOTHYROIDISM SINCE 15 YRS.
K/C/O CKD SINCE 2 YRS
P-
Head end elevation
IVF- NS@50 ml /hr
Inj. Augmentin 1.2g/ iv / bd-( day 2)
Inj. HAI s/c tid
8am- 8 units
1pm- 8 units
8pm- 8 units
T. Thyronorm 75 mcg po/od
T. Promet-xl 50 mg po/bd
T. Tetrabenazine 12.5 mg po/tid
Nebulisation with budecort -12 th hourly
Mucomist -10 th hourly
Grbs monitoring
Input and output monitoring
A 65 YR OLD FEMALE CAME TO THE THE CASUALTY WITH COMPLAINTS OF GENERALISED WEAKNESS SINCE 1 WEEK ,COUGH SINCE 4 DAYS AND INVOLUNTARY MOVEMENTS OF LT UPPER LIMB SINCE 1 DAY
H/O INADEQUATELY CONTROLLED SUGARS FROM 4 MONTHS
PT WAS EVALUATED WITH CLINICAL EXAMINATION AND AFTER NECESSARY INVESTIGATIONS, SHE WAS DIAGNOSED AS HYPERGLYCEMIA WITH CHOREA WITH DIABETIC NEPHROPATHY WITH RECURRENT URINARY TRACT INFECTION WITH IRON DEFICIENCY ANEMIA
AND FOLLOWING TREATMENT WAS GIVEN-
NBM TILL FURTHER ORDERS
INj HAI 6 U /IV/STAT AND FOLLOWED BY INSULIN INFUSION 1 ML/HR
IVF NS @ 75 ML/HR
IVF 5D @ 50 ML/HR
GRBS AND VITALS MONITORING HOURLY
USG ABDOMEN AND PELVIS SHOWED BILATERAL GRADE 1 -2 RPD CHANGES WITH RAISED ECHOGENICITY
ECG SHOWED NORMAL SINUS RHYTHM
DAY 2
InVOLUNTARY MOVEMENTS OF LT UPPER LIMB NOT REDUCED
INSULIN INFUSION CHANGED TO SUBCUTANEOUS ROUTE, HAI AND NPH GIVEN ACCORDING TO GRBS
T PROMOLET XL 50 MG PO/OD AT 8 AM ,T THYRONORM 75 MCG PO/OD AT 7 AM ,T TETRABENAZINE 12.5 MG PO/OD AT 8 AM ADDED TO THE TREATMENT
T ATENOLOL WAS WITH HELD
OPHTHALMOLOGY OPINION WAS TAKEN IN VIEW OF ANY DIABETIC AND HYPERTENSIVE RETINOPATHY CHANGES
ON FUNDUS EXAMINATION NO CHANGES WERE NOTED IN RETINA .
2D ECHO WAS DONE SHOWED-
NO RWMA ,CONCENTRIC LVH +
MILD MR+/AR+;TRIVIAL TR+
SCLEROTIC AV ,NOAS/MS
EF 58% ,RVSP=35 MMHG
GOOD LV SYSTOLIC FUNCTION
DIASTOLIC DYSFUNCTION +,NO PE
IVC SIZE (1.O7CMS) COLLAPSING
DAY 3
INVOLUNTARY MOVEMENTS WERE REDUCED COMPARED TO PREVIOUS DAY
INJ NPH WAS WITH HELD
DERNATOLOGY OPINION WAS TAKEN IN VIEW OF DRY,BROWN SCALY LESIONS ON BOTH BOTH LEGS EXTENDING TILL KNEES
AND WAS DIAGNOSED AS SNILE XEROSIS AND
ADVICED LIQUID PARAFFIN L/A BD FOR 4 WEEKS
T TECZINE 5 MG SOS
BLOOD SENT FOR CULTURE SENSITIVITY SHOWED NO GROWTH
NEUROLOGY OPINION WAS TAKEN AND ADVISED FOR MRI BRAIN
ANESTHESIOLOGIST OPINION WAS TAKEN FOR SEDATION FOR MRI
SO PAC WAS DONE I/V/O MRI UNDER SEDATION .PATIENT ATTEDERS WERE EXPLAINED ABOUT THE PROCEDURE AND POSSIBLE RISKS ASSOCIATED WITH MRI SEDATION
BUT PATIENT ATTENDERS REFUSED TO GIVE CONSENT AND MRI BRAIN WAS NOT DONE
DAY 4
INVOLUNTARY MOVEMENTS WERE REDUCED COMPARED TO PREVIOUS DAY
CULTURE AND SENSITIVITY OF URINE SAMPLE SHOWS ESCHERICHIA COLI > 100000 CFU/ML OF URINE ISOLATED AND 5-6 PUS CELLS SEEN /HPF .
SENSITIVITY SEEN TO GENTAMICIN,FOSFOMYCIN,AND AMIKACIN
INTERMIDIATE SENSITIVITY SEEN TO NITROFURANTOIN
RESISTANT TO AMOXYCLAV,CEFUROXIME,NORFLOX,COTRIMOXAZOLE,OFLAXACIN,CEFTAZIDINE,CEFEPIME,PIPERACILLIN/TAZOBACTAM.
DAY 5
SLIGHT INVOLUNTARY MOVEMENTS WERE NOTED
INSULIN DOSE WAS FIXED ,HAI 8U----8U----8U
DAY 6
REDUCED INVOLUNTARY MOVEMENTS COMPARED TO PREVIOUS DAY
DAY 7
PATIENT IS SHIFTED TO ICU AT 12 AM IN VIEW OF FALLING SATURATIONS 60% AT ROOM AIR AND FEVER 100.7F
COMPLAINTS OF SHORTNESS OF BREATH
SHE WAS PUT ON INJ AUGEMENTIN 1.2 G IV BD
NEBULIZATION WITH BUDECORT AND MUCOMIST 8TH HOURLY
INTERMITTENT CPAP
TAB NICARDIA 10MG PO/OD STAT GIVEN
PATIENT CONDITION HAS BEEN EXPLAINED TO THE ATTENDERS IN THEIR OWN UNDERSTANDABLE LANGUAGE ABOUT THE RISK ASSOCIATED WITH THE CONDITION AND IN NEW FALLING SATURATION AND POSSIBLE NEED FOR EMERGENCY INTUBATION
CHEST XRAY WAS DONE WHICH SHOWED LEFT SIDED OPACIFICATION[?CARDIOGENIC PULMONARY EDEMA ?PNEUMONIA]
DAY 8
INVOLUNTARY MOVEMENTS REDUCED COMPARED TO THE PREVIOUS DAY
PATIENT COMPLAINS OF COUGH WITH EXPECTORATION
SPUTUM FOR AFB,GRAM STAIN AND ULTURE AND SENSITIVITY SEND
PULMO OPINION WAS TAKEN I/V/O HOSPITAL ACQUIRED PNEUMONIA
AND ON EXAMINATION BILATERAL AIR ENTRY PRESENT
CREPS PRESENT AT INFRASCAPULAR REGION LEFT .RIGHT AND INTERSCAPULAR REGION AND LEFT IAA
THEY ADVISED CST,SYRUP ASCORIL LS 2TSP PO TID,NEBULIZATION WITH MUCOMIST BD,AND PLAN FOR BRONCHOSCOPY ONCE THE PATIENT IS STABLE
2D ECHO WAS DONE
RWMA PRESENT,LAD HYPOKINESIA,MILD LVH PRESENT [1.28CM]
MILD MR PRESENT,MODERATE TO SEVERE TR PRESENT WITH PAH,MODERATE AR PRESENT
SCLEROTIC AV NO AS/MS
EF 52% FAIR TO MILD LV DYSFUNCTION
DIASTOLIC DYSFUNCTION PRESENT
NO PE
IVC SIZE [1.64CM]DILATED COLLAPSING
MILD DILATED RA/LA
DAY 9
NO FEVER SPIKES SINCE PREVIOUS DAY
INVOLUNTARY MOVEMENTS ABSENT
TAB TETRABENAZINE STOPPED
COUGH WITH EXPECTORATION REDUCED COMPARED TO THE PREVIOUS DAY
INJ HAI S/C GIVEN TID 8 UNITS AT AM-1PM-8PM
SPUTUM FOR CULTURE SENSITIVITY -PSEUDOMONAS SPECIES IS ISOLATED
SENSITIVE TO PIPERACILLIN,GENTAMICIN,CIPROFLOXACIN,CEFTAZIDIME,AMIKACIN,CEFEPIME,TAZOBACTEM,MEROPENEM
DAY 10
NO FEVER SPIKES SINCE PREVIOUS DAY
INVOLUNTARY MOVEMENTS ABSENT
COUGH WITH EXPECTORATION REDUCED COMPARED TO THE PREVIOUS DAY
DAY 11
NO COMPLAINTS AND PT WAS DISCHARGED IN HEMODYNAMICALLY STABLE STATE
Advise at discharge:
INJ HAI SUBCUTANEOUS 6U----6U----6U[8AM-1PM-8PM]
TAB ECOSPIRIN -AV 75/20 PO ONCE DAILY AT 8PM
TAB HYDRALAZINE 12.5MG PO ONCE DAILY FOR 1 WEEK AT 8 AM
TAB LASIX 20MG PO/BD FOR ONE WEEK 8 AM ---------4PM
T PROMET-XL 25 MG PER ORAL TWICE DAILY AT 8 AM-----8PM
T THYRONORM 75 MCG PER ORAL ONCE DAILY AT 8 AM
LIQUID PARAFFIN LOCAL APPLICATION TWICE DAILY [MORNING AND NIGHT] FOR 4 WEEKS
SYRUP ASCORIL LS 10ML PO TID 8AM-----2PM------8PM
T TECZINE 5 MG PER ORAL SOS
STRICT DIABETIC DIET























Comments
Post a Comment