47 year old female with fever and joint pains
- Get link
- X
- Other Apps
General Medicine E-LOG Book
Final practical examination: short case
M. Sri Nithya
Hall ticket no: 1701006101
This is an online E-log book to discuss our patient de-identified health data shared after taking his/ her guardians sign informed consent
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with an aim to solve those patient clinical problem with collective current best evidence based inputs.
This E-log also reflects my patient centered online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competancy in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan.
CONSENT : An informed consent has been taken from the patient in the presence of the family attenders and other witnesses as well and the document has been conserved securely for future references.
Short case:
A 47 year old female who is tailor by occupation resident of nalgonda came to the OPD with the chief complaints of
Fever since 3 months
Facial rash since 10 days.
History of Present illness:
Patient was apparently asymptomatic 3 months back then she developed
Fever-- Insidious in onset, Intermittent -on and off ,not associated with chills and rigor. Relieved on medication . But she developed reccurent episodes of fever since then.
Then she latter developed facial rash since 10 days, which increased on exposure to sun. It was a diffuse erythematous lesion initially then became hyperpigmented. They were noted over the bilateral cheeks sparing nasolabial folds,following intake of unknown medication for abdominal pain. It is associated swelling of the left leg with erythema, and local rise of temperature.
There is no history of vomitings, abdomina pain, difficulty in breathing, palpitations or trauma.
Timeline of events--
Patient was apparently asymptomatic 11 years ago then,
She has diminision of vision 11years ago (since 2011 ).
|
And then she was certified as blind
|
Later after few months she developed bilateral knee and ankle joint pains and also pain in both the hands, for which she consulted the doctor and was diagnosed with Rheumatoid arthritis. (There was swelling associated with pain and morning stiffness for about 15mins associated with limitation of movements).Then she used medications for Rheumatoid arthritis -- diclofenac.
|
Then she was apparently asymptomatic
|
In 2021 she took covid vaccination after which she developed post vaccination joint pains for which she consulted orthopaedician. She was prescribed with some pain killers and her symptoms got relieved.
|
Then later she again complained of joint pains associated with fever 3 months ago (in March,2022).
Fever-- Insidious in onset, Intermittent -on and off ,not associated with chills and rigor. Relieved on medication . But she developed reccurent episodes of fever since then.
|
Then she latter developed facial rash since 10 days, which increased on exposure to sun. It was a diffuse erythematous lesion initially then became hyperpigmented. They were noted over the bilateral cheeks sparing nasolabial folds,following intake of unknown medication for abdominal pain.
Past History:
Patient was certified as blind in 11 years ago.
Patient presented with similar complaints of joint pain and fever in the past for which she took medication.
She is not a k/c/o diabetes, TB, asthma, epilepsy, CAD or thyroid abnormalities.
Personal History:
APPETITE:Decreased
Diet. Mixed
BOWEL AND BLADDER MOVEMENTS ; regular
SLEEP; disturbed since 10 days
ADDICTIONS : no addictions.
Family history:
There are no similar complaints in the family.
General examination:
Patient is examined in a well lit room with informed consent
Pateint is conscious, coherent,co operative well oriented to time, place and person. She is moderately built and moderately nourished.
Pallor: present
No icterus, cyanosis, clubbing,lymphadenopathy, edema.
Vitals:
PULSE :86bpm
BP:120/80mm hg
RR:16cpm
SPO2:98%at room air.
Local examination:
Face- on inspection
Erythematous and Hyperpigmented patches are present on both the cheeks and around the lips sparing the nasolabial folds.
Left lower limb swelling was present at ankle associated with redness and local rise of temperature and dorsalis pedis pulses were felt
SYSTEMIC EXAMINATION:
ABDOMEN EXAMINATION
INSPECTION:
Shape – elliptical
Flanks – full
Umbilicus –everted
All quadrants of abdomen are moving with respiration.
No dilated veins, sinuses, hernial orifices are free
No visible pulsations.
PALPATION:
No local rise of temperature and tenderness
All inspectory findings are confirmed.
No guarding, rigidity
Deep palpation- no organomegaly.
PERCUSSION:
There is no fluid thrill , shifting dullness.
Percussion of liver for liver span
Percussion of spleen- dull note
AUSCULTATION:
Bowel sounds are feeble.
CARDIOVASCULAR SYSTEM
INSPECTION:
Chest wall - bilaterally symmetrical
No dilated veins, scars, sinuses
Apical impulse seen
PALPATION:
Apical impulse is felt on the left 5th intercoastal space 1cm away from the midclavicualar line.
No parasternal heave, thrills felt.
PERCUSSION:
Right and left heart borders percussed.
AUSCULTATION:
S1 and S2 heard , no added thrills and murmurs heard.
RESPIRATORY SYSTEM
INSPECTION:
Chest is bilaterally symmetrical
Trachea – midline in position.
Apical Impulse is seen.
Chest is moving normally with respiration.
No dilated veins, scars, sinuses.
PALPATION:
Trachea – midline in position.
Apical impulse is felt on the left 5th intercoastal space.
Chest is moving equally on respiration on both sides
Tactile Vocal fremitus - appreciated
PERCUSSION:
The following areas were percussed on either sides-
Supraclavicular
Infraclavicular
Mammary
Axillary
Infraaxillary
Suprascapular
Infrascapular
Upper/mid/lower interscapular were all RESONANT.
AUSCULTATION:
Normal vesicular breath sounds heard
No adventitious sounds heard.
CENTRAL NERVOUS SYSTEM EXAMINATION.
HIGHER MENTAL FUNCTIONS:
Patient is Conscious, well oriented to time, place and person.
All cranial nerves - intact
Motor system
Right. Left
BULK
Upper limbs. N. N
Lower limbs N. N
TONE
Upper limbs. N. N
Lower limbs. N. N
POWER
Upper limbs. 5/5. 5/5
Lower limbs 5/5. 5/5
Superficial reflexes and deep reflexes are present , normal
Gait is normal
No involuntary movements
Sensory system - all sensations ( pain, touch, temperature, position, vibration sense) are well appreciated .
Provisional diagnosis:
Secondary Sjogrens syndrome with bilateral optic atrophy and left lower limb cellulitis.
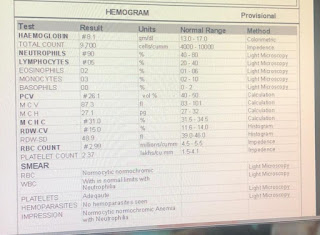
INVESTIGATIONS
,
TREATMENT
1.INJ PIPTAZ 4.5 gm IV/ TID.
2.INJ METROGYL100 ML IV/TID
3.INJ NEOMOL1GM/IV/SOS
4.TAB CHYMORAL FORTE PO/TID
5.TAB PAN 40 MG PO/ OD.
6.TAB TECZINE10 MG PO/OD
7.TAB OROFER PO/OD.
8.TAB HIFENAC-P PO/OD
9HYDROCOTISONE cream 1%on face for 1week.
- Get link
- X
- Other Apps






















Comments
Post a Comment