46 year old male patient with burning micturition, vomitings and giddiness
- Get link
- X
- Other Apps
General Medicine E-LOG Book
Final practical examination: Long case
M. Sri Nithya
Hall ticket no: 1701006101
This is an online E-log book to discuss our patient de-identified health data shared after taking his/ her guardians sign informed consent
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with an aim to solve those patient clinical problem with collective current best evidence based inputs.
This E-log also reflects my patient centered online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competancy in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan.
LONG CASE
A 46 year old male patient came to casuality with chief complaints of :
-burning micturition since 10days
-vomiting since 2days (3-4 episodes)
-giddiness and drowsiness since 1day.
History of presenting illness:
Patient was apparently asymptomatic 10 days back then he developed burning micturition, it was not associated with fever or decrease in urine output. There is no increase in urgency or frequency of micturition.
He also complained of vomiting since 2 days. The vomitus is non- projectile,non bilious,non foul smelling(3-4 episodes),containing food particles.
later he complained of giddiness and drowsiness for which he was brought to our hospital and his GRBS was recorded high value for which he was given NPH 10U and HAI 10U.
No history of fever/cough/cold
No significant history of UTIs

Past history:
10years back patient complained of polyuria for which he was diagnosed with Type 2 Diabetes Mellitus, he was started on oral hypoglycemic agents(OHA) 10years back
3years back OHAs were converted into Insulin
3years back he underwent cataract surgery
1year back he had injury to his right leg, which gradually progressed to non healing ulcer extending upto below knee and ended with undergoing below knee amputation due to developement of wet gangrene.
Delayed wound healing was present- it took 2months to heal
Not a k/c/o Hypertension, Epilepsy,Tuberculosis, Thyroid
Not on any medication
No history of blood transfusion
Personal history:
Appetite- normal
Diet - Mixed
Bowel and bladder- Regular, burning micturition present
Sleep- Adequate
Habits/Addiction:
Alcohol-
Not consuming alcohol since 1 yr.
Previously (1yr back) Regular consumption of alcohol, about 90mL whiskey consumed almost daily.Also 1 month on & off consumption pattern previously present
Family history:
Not significant
General Examination:
Patient was examined in a well lit room with informed consent.
Patient is conscious, coherent, co-operative, well oriented to time, place and person.
Pallor- present
No- icterus,cyanosis,clubbing,koilonychia, lymphadenopathy
No dehydration.
Vitals @ Admission:
BP: 110/80 mmHg
HR: 98 bpm
RR: 18 cpm
TEMP: 99F
SpO2: 98% on RA
GRBS: 124 mg/dL
SYSTEMIC EXAMINATION:
S1 and S2 heard , no added thrills and murmurs heard.
RESPIRATORY SYSTEM
INSPECTION:
Chest is bilaterally symmetrical
Trachea – midline in position.
Apical Impulse is not appreciated
Chest is moving normally with respiration.
No dilated veins, scars, sinuses.
PALPATION:
Trachea – midline in position.
Apical impulse is felt on the left 5th intercoastal space.
Chest is moving equally on respiration on both sides
Tactile Vocal fremitus - appreciated
PERCUSSION:
The following areas were percussed on either sides-
Supraclavicular
Infraclavicular
Mammary
Axillary
Infraaxillary
Suprascapular
Infrascapular
Upper/mid/lower interscapular were all RESONANT.
AUSCULTATION:
Normal vesicular breath sounds heard
No adventitious sounds heard.
CENTRAL NERVOUS SYSTEM EXAMINATION.
Higher mental functions test:
Pt is having altered sensorium
Slurred speech
Not Orientated to time place person.
Memory couldn't be elicited as pt is in altered sensorium
Cranial nerves : intact
Motor system :
1, Bulk : right. Left
Upper limb normal. Normal
Lower limb. thigh -N. Normal
Below knee amputated on R side
2, Tone :
Upper limb. Normal. Normal
Lower limb. Normal. Normal
3.Power :
Neck:. Normal
Trunk:. Normal
Upper limb 5 5
Lower limb 5 5
4, Reflexes
Right Left
Biceps 2+. 2+
Triceps 2+ 2+
Supinator. 2+ 2+
Knee 2+. 2+
Ankle 2+. 2+
Planter reflex Amputated flexion
Sensory system : normal
Meningeal signs : negative
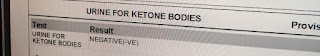
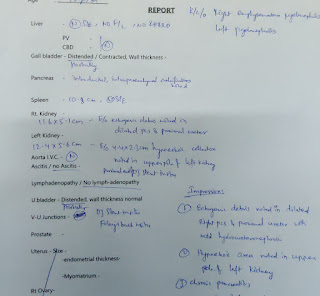
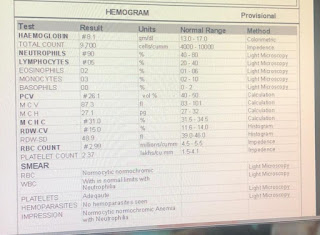
Investigations:
On admission (19.5.22)
X ray KUB

CT Scan

Renal function tests:
Ultrasound report abdomen and pelvis
 |
20.05.22
LDH- 192
24hr Urinary protein- 434
24hrs Urinary creatinine- 0.5
Culture report: Klebsiella Pneumonia positive
Pus cells
21.5.22
Hemoglobin- 6.8g%
TLC- 22,500cells/cumm
Platelets- 1.4lakhs/cu.mm
Urea- 155mg/dl
Creatinine- 4.7
Uric acid- 7.1
Phosphorus- 2.0
Sodium- 126
Potassium- 2.6
Chloride- 87
22.5.22
Hemoglobin- 7.2
TLC- 17,409
Platelet count- 1.5
Urea- 162
Uric acid- 5.0
Sodium- 125
Chloride- 88
23.2.22
25.5.22
27.5.22
Hb- 7gm%
TLC- 22,000
Platelet count- 26,000
Urea- 144
Creatinine - 4.8
Uric acid-9.1
Phosphorus- 4.8
Sodium- 135
Potassium- 4.3
Chloride- 98
Fasting blood sugar- 149
29.5.22
Hb- 6.4
TLC- 14,700
Platelet count- 6000
Urea - 149
Creatinine- 4.4
Uric acid- 9.2
Provisional Diagnosis:
Right emphysematous pyelonephiritis and left acute pyelonephiritis, encephalopathy secondary to sepsis.
H/o of Type 2 Diabetes mellitus since 10years
Treatment:
Day 1 to Day 3:
INJ. MEROPENEM 500mg IV BD
INJ. ZOFER 4mg IV TID
INJ. PAN 40mg IV OD
IV Fluids- NS,RL @ 100 mL/hr
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
RT feeds- 2nd hrly 100 mL water
Day 4
INJ. MEROPENEM 500mg IV BD
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. KCl 2 Amp in 500 mL NS over 4.5 hrs infusion
IV Fluids- NS,RL @ 100 mL/hr
SYP. POTCHLOR 10 mL in 1 glass of water TID
SYP. MUCAINE GEL 10 mL PO TID
7 point profile
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
RT feeds- 2nd hrly 100 mL water
Day 5 to Day 10:
INJ. MEROPENEM 500mg IV BD (Day 6)
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. LASIX 40 mg IV BD
IV Fluids- NS,RL @ 100 mL/hr
SYP. MUCAINE GEL 10 mL PO TID
GRBS 7 point profile
INJ.HAI SC TID ACC to GRBS
TAB.DOLO 650 mg SOS
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
Day 11:
INJ. COLISTIN 2.25 MU IV OD(Day 4)
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. LASIX 40 mg IV BD
IV Fluids- NS,RL @ 100 mL/hr
SYP. MUCAINE GEL 10 mL PO TID
GRBS 7 point profile
INJ.HAI SC TID ACC to GRBS
TAB.DOLO 650 mg SOS
Day 12:
SDP Transfusion done I/v/o low platelet count
Pre transfusion counts:
Hb:6.2 g/dL
TLC:14700
PLt:6000
Post transfusion counts:
Hb:6.4
TLC:13700
PLt:50000
- Get link
- X
- Other Apps














Comments
Post a Comment