15 year old male with left sided chest pain, breathlessness.
Final practical examination: Long case
M. Sri Nithya
Hall ticket no: 1701006101
This is an online E-log book to discuss our patient de-identified health data shared after taking his/ her guardians sign informed consent
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with an aim to solve those patient clinical problem with collective current best evidence based inputs.
This E-log also reflects my patient centered online learning portfolio
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competancy in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan.
CONSENT : An informed consent has been taken from the patient in the presence of the family attenders and other witnesses as well and the document has been conserved securely for future references.
Long case:
15 year old male patient who is a student by occupation came to the OPD with the chief complaints of
Chest pain in the left side since 3 months
Difficulty in breathing since 15 days.
History of Present illness:
Patient was apparently asymptomatic 3 months ago then he developed chest pain on the left side which is insidious in onset, gradually progressive and is of dragging type,non radiating. It is aggravated during walking or doing some work and relieved on taking rest.
Patient complaints of difficulty in breathing since 3 months which was intermittent initially and is increased during the past 15 days.(MRCC- grade 1) Breathlessness is present after waking up from bed and then it decreases after some time. It is aggravated when the patient lies down in left lateral position and relieved when the patient lies down in right lateral position and upon sitting.
It was also associated with cough since 3 months which is intermittent and not associated with sputum.
Associated with fever since 3 months which is intermittent in nature and is of low grade, not associated with chills and rigor. It subsides on its own and patient did not use any medications.
Patient also complaints of fatigue since 2 months.
With these complaints he went to the local hospital and also consulted orthopaedician where no abnormality detected.
Later he went to another hospital where his chest x-ray and CT scan were done. Then he was admitted in the hospital for 7-10 days where he was given O2 supplementation and saline infusion. Then his symptoms got relieved and he was discharged.
After 10 days of discharge, he again developed chest pain on the left side, so he consulted another doctor where he was diagnosed with hydropneumothorax.
Chest pain and difficulty in breathing increased during the last 15 days hence he came to our hospital.
There is no history of PND,orthopnea,palpitations,vomitings, hempotysis, or trauma.
Past history:
Time line of events--
Patient is not a known case of HTN, DM, TB, asthma, epilepsy, CAD and any thyroid abnormalities.
Personal history:
Appetite - normal
Diet - mixed
Bowel and bladder- normal micturition , complaints of constipation since 2 years. Passage of hard stools for every 3-4 days.
Sleep- adequate.
Addictions- No
Allergies - No
Family history:
No significant family history.
General examination:
Patient is examined in a well lit room with informed consent
Pateint is conscious, coherent,co operative well oriented to time, place and person. he is moderately built and moderately nourished.
Pallor: present
No icterus, cyanosis, clubbing, generalised lymphadenopathy, edema.
Vitals:
PR- 76bpm
RR- 18 cpm
BP-110/70 mmhg measured in sitting postion in the right arm
Temperature -98.6 F
Spo2- 96% on room air
Systemic examination -
Respiratory system
Inspection:
Shape - elliptical
No tracheal deviation
Chest bilaterally symmetrical
Expansion of chest- normal
Breathing is abdominal thoracic
Use of accessory muscles - no
No dilated veins,pulsations,scars, sinuses.
No drooping of shoulder.
Palpation:
There is no local rise of temperature and tenderness
All the Inspectory findings are confirmed
trachea- present centrally
Apex beat- 5th intercoastal space, 1 cm lateral to midclavicular line.
Vocal fremitus- decreased on left side in infraaxillary and infrascapular region.
Measurements:
Anteroposterior length: 20cm
Transverse length: 28cm
Right hemithorax: 38cm
Left hemithorax: 36cm
Circumference: 74cm
Percussion:
Dull note heard at the left infraaxillary and infrascapular areas
Liver dullness from right 5th intercostal space
Auscultation:
Bilateral air entry present.
Vesicular breath sounds heard.
Decreased intensity of breathe sounds heard in infrascapular region and absent breathe sounds in left infraxillary area.
Vocal resonance: decreased in left infraaxillary and infrascapular areas.
ABDOMEN EXAMINATION
INSPECTION:
Shape – scaphoid
Flanks – full
Umbilicus –everted
All quadrants of abdomen are moving with respiration.
No dilated veins, sinuses, hernial orifices are free
No visible pulsations.
PALPATION:
No local rise of temperature and tenderness
All inspectory findings are confirmed.
No guarding, rigidity
Deep palpation- no organomegaly.
PERCUSSION:
There is no fluid thrill , shifting dullness.
Percussion of liver for liver span
Percussion of spleen- dull note
AUSCULTATION:
Bowel sounds are normal.
CARDIOVASCULAR SYSTEM
INSPECTION:
Chest wall - bilaterally symmetrical
No dilated veins, scars, sinuses
There is no precordial bulge
Apical impulse is present in left 5 th intercoastal space.
PALPATION:
Apical impulse is felt on the left 5th intercoastal space 2cm away from the midline.
No parasternal heave, thrills felt.
PERCUSSION:
Right and left heart borders percussed.
AUSCULTATION:
S1 and S2 heard , no added thrills and murmurs.
CENTRAL NERVOUS SYSTEM EXAMINATION.
HIGHER MENTAL FUNCTIONS:
Patient is Conscious, well oriented to time, place and person.
All cranial nerves - intact
Motor system
Right. Left
BULK
Upper limbs. N. N
Lower limbs N. N
TONE
Upper limbs. N. N
Lower limbs. N. N
POWER
Upper limbs. 5/5. 5/5
Lower limbs 5/5. 5/5
Superficial reflexes and deep reflexes are present , normal
Gait is normal
No involuntary movements
Sensory system - all sensations ( pain, touch, temperature, position, vibration sense) are well appreciated .
Provisional diagnosis:
Mild left sided hydropneumothorax
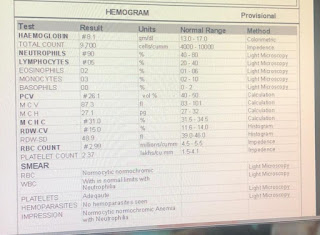
Investigations:
Chest x- ray: Resolved hydropneumothorax
USG report:
ECG:
Bronchoscopy:
Treatment:
On admission (4-6-2022)
1. High flow oxygen inhalation facemask
2. Plan for ICD placement
3. Monitor vitals.
4. ICD should be placed immediately for worsening of SOB.
5.Monitor vitals.
10-6-2022
Patient was sent for bronchoscopy.
After the procedure , patient was advised with-
1.NBM for 2 hours.
2. Sips of water was taken at 12:00 noon.
3. Soft diet was started at 2:00 pm.
4: T. PCM 650 mg
5. Inj. Neomol i. V BD, (PCM infusion)
6. Neb. With Duolin tid, budecort, mucomyst.
7. Chest physiotherapy.
8. Monitor vitals .
On 11-6-2022
Monitor vitals

















Comments
Post a Comment