35 years old female with dermatomyositis
- Get link
- X
- Other Apps
A 35yr old female with cough and dyspnea
This is an online E log book to discuss our patient's de-identified health data shared after taking her guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
M. Sri Nithya
Roll.no 75.
IDENTIFICATION :
The privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whatsoever.
CONSENT : An informed consent has been taken from the patient in the presence of the family attenders and other witnesses as well and the document has been conserved securely for future references.
ACKNOLEDGEMENTS:
https://61tejarshini.blogspot.com/2022/01/medicine-case-discussion.html
https://rhea9895.blogspot.com/2022/01/29-years-old-female-with-co-joint-pains.html
https://nikitha0510.blogspot.com/2022/03/dermatomyositis.html
I am extremely grateful toDr. Saicharan Kulkarni sir (PG) for guiding me through the case and helping me build this blog
March 15,2022
CASE:
35 years old female homemaker by occupation came to the General Medicine OPD with the CHIEF COMPLAINTS of dyspnea in rest since 4 days
cough since 4 days
B/L joint pains associated with edema over legs from knee to ankle joint including dorsum of foot since 4 days
High grade fever since 1 day
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 12 months ago.
- Then she developed symmetrical bilateral joint pains in the knees which was insidious in on set, gradually progressive, no aggravating factors and relieved on medication i.e. Tab. HYDROXYCHLOROQUINE 200 mg
- Associated with morning stiffness.
- Around the same time she developed itching over neck and upper chest area. As a result of the itching, the area was initially red and turned black.
- C/O Alopecia since 12 months. It was gradually progressive leading to severe hair loss over the past 12 months. Associated with thinning of hair.
- C/O bilateral pitting type of pedal Edema and Edema over the dorsal aspect of hands since 12 months
- C/O generalized pain.
- C/O Difficulty in walking.
- C/O distal muscle weakness manifested in the form of difficulty in mixing food, eating with hands, buttoning-unbuttoning of shirt,
- C/O proximal muscle weakness manifested in the form of : difficulty in getting up from squatting position, getting objects present at a height.
- C/O vaginal discharge since 10 months. It was initially curdy white which later changed to watery discharge. Associated with itching.
- C/O weight loss of 4 kg over the last 10 months.
- C/O oral ulcers and genital ulcers since 10 months.
- C/O Dyspnea on exertion (NYHA- 3), gradually progressive since 6 months.
- She visited many local RMPs, received pain killers as there is no improvement, she visited a health center 2 months back
- Presence of facial hair since 1 month
- C/O Dyspnea on rest (NYHA- 4), gradually progressive since 4 days
- h/o cough since 4 days associated with sputum.
- -h/o fever since 4 days
- C/o throat pain since 4 days
Past History:
Not a K/O/C of HTN, BA, epilepsy, Asthma, CVA, CAD.
Had similar complaints in the past 2 months.
Diagnosed with diabetes after coming to the hospital on 15th March
Menstrual History
AOM- 11 years
3/25-28, regular , no pains, no clots.
Marital History
ML- 14 years, NCM
Primary infertility (Nulligravida)
Has recently adopted a girl from her sister-in-law.
Family History
No similar complaints in the family .
DAILY ROUTINE OF THE PATIENT :
The patient lives in a family of 3 which constitutes her husband ,her mother in law and herself . They follow Islam.
A usual day in her life :
4.40 am : wakes up and bathes
5.00 am : Prayer
5.15 am : She doesn't sleep but lies on her bed and rests for another one or two hours .
7.30 am : washes dishes from the last day, washes clothes, makes the morning tea for herself and her family members
9.00am : gets food ready for her husband who goes out for work after breakfast
9.30 am : Serves breakfast for her mother in law and herself
Rests for a while
11.00 am : Prepares for the day's cooking
Rests for a while
12.00 noon : cooks for the day
1.00 pm : Serves lunch for her husband who comes back during afternoon
2.00 pm : Serves lunch for her mother in law and herself
3.00 pm : Rests
4.00 pm : Prayer
5.00 pm : Makes tea for everyone in the house
In the evening mostly all of them sit down and watch television
7.00 pm : Preparations for dinner.
8.30 pm : Serves dinner for the family and then for herself
10.00 pm : Sleeps
Personal History
Diet- Mixed
Appetite- Decreased
Sleep- Inadequate since 12 months. Wakes at 2 AM-3AM because of pain in legs.
Bowel and bladder habits- Irregular
C/O loose stools for 4 days followed by constipation for 3 days since 8 months.
No addictions
No known drug allergies .
Following are the clinical images when she visited health center 2 months back:
Single erythematous macule noted over the right loin (Holster sign).
Pigmentation of B/L extensor surfaces of PIP, DIP joints noted (Gottron's papules).
Treatment given 2 months back:
Tab.wysolone 50mg po/od
Syp.mucaine 10ml/po/tid
Tab.ultracet 1/2 po/QIT
Candid cream for L/A is advised.
Patient was referred to other health center for muscle biopsy.
Patient went to health center, her ANTI NUCLEAR ANTIBODY IMMUNOFLUOTESCENCE showed homogeneous pattern. Intensity 4+ associated antigens involved-ds DNA, histones.
HRCT WAS DONE ON 21/1/22
IMPRESSION: Few patchy areas of ground glass opacities in peri bronchovascular distribution-s/o pneumonitis .Corads-4
She didn't undergo muscle biopsy as the doctors there advised it is not necessary
THEY PRESCRIBED:
TAB.CALTEN
TAB.AUGMENTIN
TAB.NAPROXEN SODIUM
TAB.FOLVITE
CANDID CREAM
TAB.WYSOLONE
TAB.ESOMEPRAZOLE
TAB.SODIUM ALENDRONATE WEEKLY ONCE.
- She is moderately built and moderately nourished
- Pallor- present
- No icterus, cyanosis, clubbing, lymphadenopathy
- Pedal Edema- present
O/E:
Patient images after treatment of 2 months
DEVELOPED FACIAL HAIR GROWTH POSSIBLY DUE TO TREATMENT WITH WYSOLONE (CORTICOSTEROID)
WHITE PATCH OVER TONGUE AND TONSILS
Vitals:
Temperature- Afebrile
BP- 150/100 mm Hg
PR- 114bpm
RR- 30cpm
SpO2- 93% @ RA
Fever charts:
SYSTEMIC EXAMINATION
Respiratory system examination:
A. Inspection
- Symmetrical chest
- Decreased air entry on right side
- V shaped line seen below the neck
- No dilated veins or scars visible
B. Palpation
- No lymph nodes palpable
- Tactile vocal fremitus increased In lower part of right lung
- Trachea centrally positioned
- Apex beat felt at the 5th intercostal space along the mid-clavicular line
C. Percussion
Dull note over right infrascapular region, all other regions are resonant
D. Auscultation
- Normal vesicular breath sounds heard
- Decreased air entry in right infrascapular ,right mammary and inframammary areas
OTHER SYSTEMS:
CNS-
HIGHER MENTAL FUNCTIONS:Normal
P/A- Soft and non tender, Bowel sounds heard
PROVISIONAL DIAGNOSIS:
DERMATOMYOSITIS WITH RIGHT LOWER LOBE CONSOLIDATION AND PULMONARY NOCARDIOSIS.
CHEST X RAYS:
January 2022:
15 March 2022:
26th March 2022:
28th March 2022:
INFERENCE: RIGHT LOWER LOBE CONSOLIDATION.
ECG:
IMPRESSION: RIGHT RENAL CORTICAL CYST WITH WALL CALCIFICATION.
2D ECHO ON 15/3/22:
EF-60%
MILD TR WITH PAH
TRIVIAL AR/MR
GOOD LV SYSTOLIC FUNCTION
NO DIASTOLIC DYSFUNCTION.
PFT REPORT ON 16/3/22:
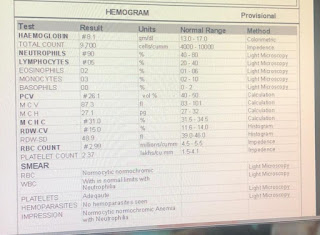
CBP:
HB:9.9
TLC:9600
N/L/E/M:90/6/2/2
PCV:29.2
MCV:82
MCH:27.8
MCHC:33.9
RBC:3.56
PLT:1.77
LFT
TB-0.82
DB-0.24
AST-16
ALT-18
ALP:147
ALB-2
A/G-0.62
RFT
SR.UREA-29
SR.CREAT-0.9
NA+-137
K+-3.5
CL-:98
BGT
AB POSITIVE
RBS
312 MG/DL
COMPLETE URINE EXAMINATION:
- ALBUMIN-TRACE
- SUGAR-NIL
- PUS cells-2-3
- EPITHELIAL cells: 2-3
SPUTUM CULTURE on 29.03.2022:
Since patient was having cough with sputum which was moderate in amount and whitish yellow in colour, sputum was sent for culture.
Presence of branching and filamentous thin, long, slender AFB resembling Nocardia seen under microscope from sample of both lungs.
Impression : NOCARDIA SPECIES
BRONCHOSCOPY 29.03.22
Sensitive antibiotics were started but suboptimal response was obtained hence a doubt was raised if the Nocardia was cultured due to some contamination of the plates , and hence BRONCHOALVEOLAR LAVAGE was done.
https://m.youtube.com/watch?v=Q4L1HcPtI9o&feature=youtu.be
TREATMENT:
1.T.SEPTRAN DS TID 1--1--1
2.TAB.FLUCONAZOLE 150 MG OD
3.OINT.CANDID MOUTH PAINT IN ORAL CAVITY
4.TAB.WYSOLONT 50 MG OD 1--X--X
5.TAB.FOLIC ACID 5 MG ONCE A WEEK.
TREATMENT 31.03.22
1.INJ.MEROPENEM 500MG IV BD(Day- 4 )
2.TAB.SEPTRAN DS TID (DAY -13)
3.TAB.DOXY 100MG PO BD (DAY-7)
4.OINT. CANDID MOUTH PAINT IN ORAL CAVITY
5.TAB.AZATHIOPRINE 50 MG OD(DAY-8)
6.TAB.FOLIC ACID 5 MG ONCE WEEKLY
7.SYP.GRILINCTRUS BM
8.TAB.METFORMIN 500MG OD
9.ZYFER GEL FOR L/A
10.TAB.DOLO 650MG PO TID
11.TAB.WYSOLONE 50 MG OD
- Get link
- X
- Other Apps




.jpg)

































Comments