60 year old male patient with fever, shortness of breath and swelling of right lower limb
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with an aim to solve those patient clinical problem with collective current best evidence based inputs.
This E-log also reflects my patient centered online learning portfolio.
Your valuable inputs on comment box is welcome
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competancy in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan
A 60 year old male patient from dhamera village came to casuality with chief complaints:
Fever since 8 days
Right LL swelling and redness since 7 days
SOB grade 2----> 4 since 6 days
History of presenting illness:
Patient was apparently asymptomatic 8 days back and then he developed fever which was low grade, intermittent, relieved on taking medication and not associated with chills and rigor.
Patient was a farmer 7 years ago but now his sons take care of his land , since then he doesn't do any farming work. His wife passed one year ago, since then he lives alone at his home. He used to get knee pain frequently for which he used to consult nalgonda hospital and the pain used to get relieved after taking medications.
He has back pain from nape of neck to lower back which is of dragging in nature 3 days before the onset of swelling. It used to relieve on taking medications.
Then he developed leg pain for which he applied ointment over right foot 3days back and later he developed redness and swelling over right foot.
No history of trauma or injury.
He has SOB (grade 2 which later progressed to grade 4) since 6 days.
No orthopnea or PND or chest pain or palpitations.
With these complaints they went to outside hospital and on presentation to the outside hospital vitals are spO2-74% on RA with,
BP 70/40 and
Decreased urine output.
All necessary Investigations were done and he was treated with IV Antibiotics, IV antacids, IV nebulization, IV ionotropes, IV multivitamins. He was put on CPAP, and his conditions was explained and was advised for hemodialysis. But patient attendees was not willing for further investigation and wanted to refer to our hospital.
Past history ;
Not a k/c/o Dm,HTN,CAD,asthma,TB
Family history: No similar complaints in the family and no significant history
Personal history:
Diet is mixed
Appetite is normal
Sleep is Adequate
Bladder and bowel are regular
Additions: no
Allergy: not known allergy
General Examination:
Patient is examined in a well lit room.
Patient is unconscious, Not oriented to time, place and person. Patient is well built and moderately nourished.
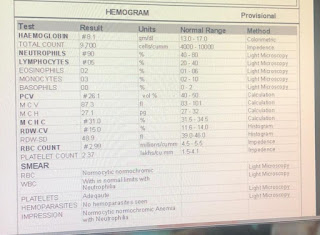
Pallor is present,
No icterus, cyanosis, clubbing, koilonychia, lymphadenopathy, edema is seen on right lower limb which is mild and non pitting type.
Vitals:
Temperature: 100 F
Pulse rate: 95 beats per minute with normal rhythm,volume and character.
Respiratory rate: 25 per minute
Blood pressure: 100/70 mmHg in supine position
SPO2: 100% at 10 L of O2
Systemic Examination:
Respiratory system:
UPPER RESPIRATORY TRACT:
Oral hygiene ,Halitosis, oral thrush, postnasal drip, pharyngeal deposits, tonsils, dental caries, deviated nasal septum with turbinate hypertrophy, nasal polyps, sinus tenderness cannot be assessed.
LOWER RESPIRATORY TRACT:
INSPECTION:
Chest is symmetrical,normal in shape,
Trachea - midline,
tracheal movement during inspiration- normal
There is no supraclavicular/infraclavicular hollowing, intercostal fullness/indrawing/retraction/widening.
No Sinuses, scars, dilated veins, nodules
Movement with respiration- normal
PALPATION:
Temperature- no local rise of temperature
Trachea – midline
No Intercostal widening/crowding of ribs, rickety/scorbutic rosary, Intercostal tenderness, subcutaneous emphysema
No dilated veins – direction of flow, nodules
Chest movement- normal
Tactile Fremitus, Friction Fremitus, Vocal Fremitus- cannot be assessed.
PERCUSSION:
Right/Left
Dullness is seen in inframammary and midaxillary area on both sides.
AUSCULTATION:
There is decreased bilateral air entry.
Breath sounds-
B/l crepts present in IAA and ISA
3. Vocal Resonance- cannot be assesed.
CVS examination:
S1,S2 are heard normally.
P/A: soft and non tender.
CNS exam: unconscious.
Clinical Images:
Chest x ray:
MRI:
ECG-
Day 1-
2d echo report:
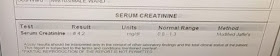
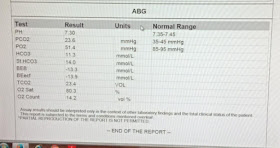
ABG at 6am:
ABG at 1.40 pm:
Fever chart
Diagnosis:
Sepsis secondary to right lower limb cellulitis
?Moderate ARDS (PaO2/FiO2= 100)
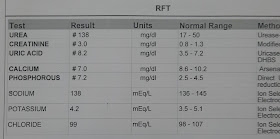
Pre renal AKI and ? Ischemic hepatitis
? Lumbar spondylosis (L2 to L5).
Treatment:
1. Propped up posture
2. O2 inhalation at 8 to 10 L/min
Maintain spO2 > 90%
3. BIPAP 4th hourly
4. Inj. PIPTAZ 4.5g /IV /stat
To inj. PIPTAZ 2.25g IV QID
5. INJ. CLINDAMYCIN 600MG IV TID
6. INJ. PAN 40MG IV OD
7. INJ. ZOFER 4MG IV BD
8. INJ. PCM 1G IV SOS
9. T. PCM 650MG PO TID
10. IVF NS and RL at U.O + 50 ml/hr
11. INJ. NORADRENALINE at 8 ml/hr to increase or decrease acc to MAP > 65 MMHG
12. INJ. LASIX 20MG PO OD
Update: day 2
Post debridememt right Lower limb
Drugs used -
Post intubation:
Abg:
On 9/1/22
Day 3
S: NO fever spikes
O: pt intubated and is on mechanical ventilator
ACMVPC mode
Peep 7
Fio2 100
I:E 1:2
Pt is still on ionotropes noradrenaline @16ml/hr
Vasopressin @1.5ml/hr
Pt sedated and paralysed, on dexmedetomidine 10ml/hr
Atracurium 5ml/hr
intermittent regaining of consciousnes
B/L pupil reacting to light
Vitals
Bp : 100/70mmhg
PR : 82 bpm
Spo2 : 100% on fio2 100
Grbs:121
Systemic Examination
Cvs : s1s2+
Rs: b/L basal crepts +
P/A : soft,bs+
Ecg
Cxr
Treatment:
Rt feeds 200ml milk +free water 2nd hourly
IV fluids @75ml/hr
1. Propped up posture
2. O2 inhalation at 8 to 10 L/min
Maintain spO2 > 90%
3. BIPAP 4th hourly
4. Inj. PIPTAZ 4.5g /IV /stat
To inj. PIPTAZ 2.25g IV QID
5. INJ. CLINDAMYCIN 600MG IV TID
6. INJ. PAN 40MG IV OD
7. INJ. ZOFER 4MG IV BD
8. INJ. PCM 1G IV SOS
9. T. Paracetomol 650MG PO TID
10. IVF NS and RL at U.O + 50 ml/hr
11. INJ. NORADRENALINE at 8 ml/hr to increase or decrease acc to MAP > 65 MMHG
12. INJ. LASIX 20MG PO OD
On 10/01/22
S :fever spike observed
O: pt intubated and is on mechanical ventilator
ACMV pC mode
Peep 7
Fio2 60%
I:E =1:2
Pt is still on ionotropes noradrenaline @16ml/hr
Vasopressin @1.5ml/hr
Vitals:
Bp : 110/70mmhg
PR : 102 bpm
Spo2 : 100% on fio2 60%
Rr :14/min
Systemic Examination :
Cvs : s1s2+
Rs: b/L basal crepts +
P/A : soft,bs+
Treatment:
Rt feeds 200ml milk +free water 2nd hourly
IV fluids @75ml/hr
1. Propped up posture
2. O2 inhalation at 8 to 10 L/min
Maintain spO2 > 90%
3. BIPAP 4th hourly
4. Inj. PIPTAZ 4.5g /IV /stat
To inj. PIPTAZ 2.25g IV QID
5. INJ. CLINDAMYCIN 600MG IV TID
6. INJ. PAN 40MG IV OD
7. INJ. ZOFER 4MG IV BD
8. INJ. PCM 1G IV SOS
9. T. Paracetomol 650MG PO TID
10. IVF NS and RL at U.O + 50 ml/hr
11. INJ. NORADRENALINE at 8 ml/hr to increase or decrease acc to MAP > 65 MMHG
12. INJ. LASIX 20MG PO OD

































Comments
Post a Comment