Name- M. Sri Nithya
Roll. No- 75
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
Following is the view of my case: (history as per date of admission)
38 year old male patient came to the casuality with the chief complaints of
Decreased appetite since 3-4 months
Fever since 3 months(on and off) aggravated during last 10 days
Decreased urine output since 15 days
History of present illness:
Patient was apparently asymptomatic 4 months ago then
He developed decreased appetite and
Fever since 3 months which is insidious in onset, gradually progressive, intermittent, aggravated during last 10 days. It is associated with chills not associated with rigor. It relieved on medication.
There is decreased urine output since 15 days.
There is no history of blood in urine, facial puffiness,pedal edema, pain in the abdomen, chest pain, shortness of breath, palpitations.
Past History:
There is no history of TB, asthma, hypertension, diabetes mellitus, cardiovascular diseases.
No H/O previous surgeries.
Personal history
Appetite- normal
Diet -mixed
bowel and bladder -regular
Sleep- adequate
Addictions-He is a chronic smoker since 10 years
He is chronic alcoholic since 15 years
No known allergies.
Family history
No significant family history.
General examination
Patient is examined in a well lit room with informed consent.
He is conscious, coherent, co-operative,well oriented to time,place and person.
He is moderately built and moderately nourished.
Pallor - present
Icterus - absent
Cyanosis - absent
Clubbing - absent
Lymphadenopathy - absent
Edema - absent
Vitals:
Temperature-afebrile
Heart rate-90 beats/min
Blood pressure-110/70 mmHg
Respiratory rate-22cycles/min
SPO2-98% at room air.
Grbs- 140 mg%
SYSTEMIC EXAMINATION:
CVS: S1 and S2 heard
No added thrills, murmurs
RESPIRATORY SYSTEM:
Trachea is central,
Normal vesicular breath sounds were heard on both sides.
There is no dyspnoea or wheeze.
CENTRAL NERVOUS SYSTEM:
Level of consciousness : conscious to time, place, person
Speech: normal
Cranial nerves -Normal
Motor and sensory: normal
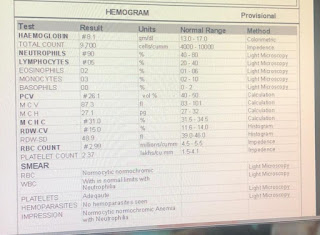
INVESTIGATIONS
Diagnosis: Acute kidney injury on CKD. secondary to post renal obstruction ( ureteric obstruction) with B/l hydronephrosis.
Treatment:
Inj. Lasic 40 mg I.V OD
Tab. Nodosis 500 mg BD
Tab. Shelcal ct OD
Tab. Orofer BD
Inj. Erythropoeitin 4000 IU S/c weakly once
Inj. Iron sucrose 1ampoule 500 ml















Comments
Post a Comment